Every year, tens of thousands of patients in the U.S. are harmed or die because of preventable medication errors. It’s not because pharmacists are careless. It’s because the system is overloaded. A single pharmacist might handle 200+ prescriptions in a day. Each one requires checking the right drug, dose, patient, allergies, interactions, and expiration date-all while juggling phone calls, insurance issues, and staff questions. Human error isn’t a failure of character. It’s a failure of design.
How Pharmacy Workflows Used to Work
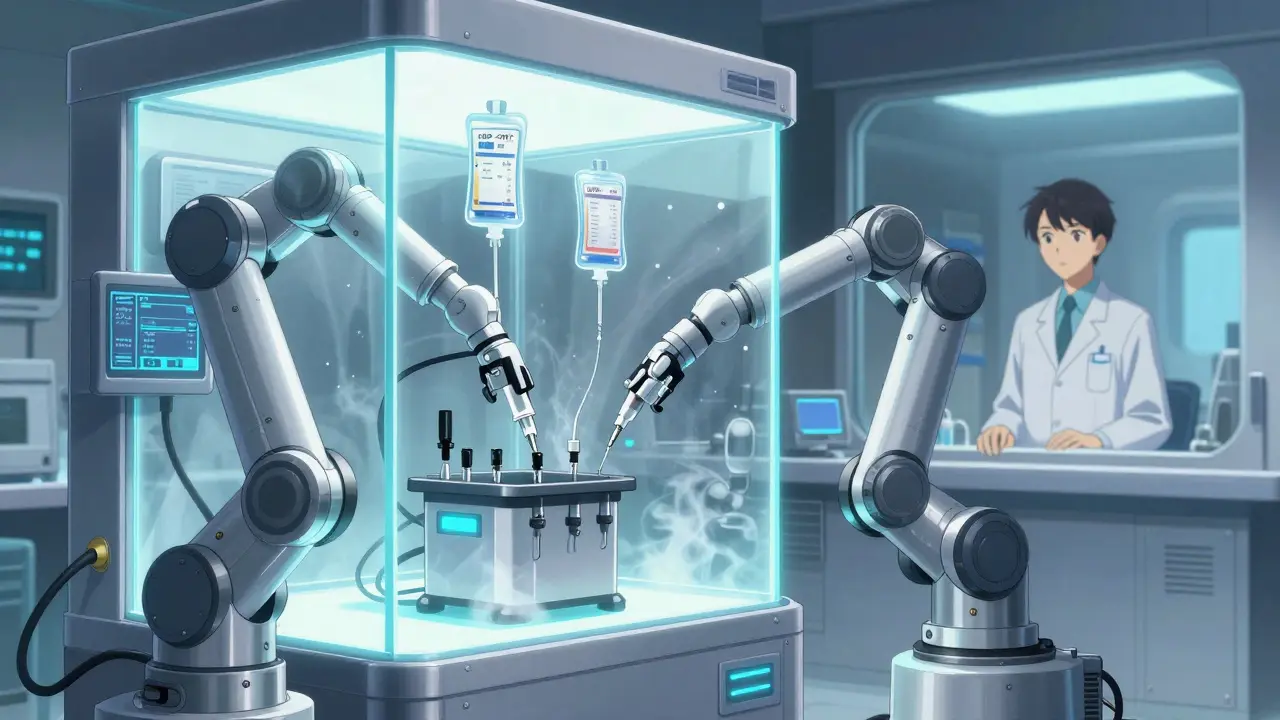
Ten years ago, most community and hospital pharmacies ran on paper and memory. A prescription came in-either printed, faxed, or electronically. The pharmacist read it, pulled the bottle from the shelf, counted pills, labeled it, and checked it against the order. Then a technician or another pharmacist did a second check. Sometimes, they didn’t. Sometimes, the label was smudged. Sometimes, the patient’s allergy wasn’t in the system. Sometimes, the wrong strength was picked because the bottles looked alike. The biggest risks came from high-volume tasks: IV compounding, pediatric doses, and overnight shifts. A 2015 study found that IV preparation errors occurred in nearly 1 in 8 doses in some hospitals. That’s not because the staff was untrained. It’s because mixing chemotherapy drugs by hand, under time pressure, with multiple steps and sterile requirements, is asking for mistakes.What Changed: The Rise of Automated Workflow Systems
Around 2005, pharmacies started adopting digital tools to fix these problems. Not just electronic prescriptions-but full pharmacy workflow systems. These aren’t fancy robots in sci-fi movies. They’re practical, real-world tools built by pharmacists for pharmacists. Today’s systems combine three key technologies:- Barcode scanning at every step: from receiving the script to handing the medicine to the patient.
- Automated dispensing cabinets like BD Pyxis™ that only release the right drug when the right person scans their badge and the right patient ID is entered.
- Software that checks everything: drug interactions, allergies, duplicate therapy, dosing for age or kidney function-all in real time, before a pill leaves the counter.
How Error Prevention Works in Practice
Let’s say a doctor prescribes 10 mg of warfarin for a 78-year-old woman. The system pulls up her profile: she’s on amiodarone, has kidney issues, and had a recent bleed. The software flags it immediately: “High risk of bleeding. Suggested dose: 2.5 mg.” The pharmacist reviews it, calls the doctor, and the dose is changed. No patient hurt. No lawsuit. No tragedy. That’s not luck. That’s the system working. Here’s how the workflow flows now:- Prescription is received electronically from the doctor’s system.
- Software checks for allergies, interactions, and correct dosing based on patient data in the EHR.
- Pharmacist reviews the alert and approves or adjusts the order.
- Automated dispensing unit releases the correct bottle only after scanning the patient’s barcode and the pharmacist’s badge.
- Robot or technician prepares IV bags with precise measurements-no manual measuring.
- Final check: barcode scan of the medication and patient wristband before delivery.
Types of Systems Used Today
Not all pharmacy workflow systems are the same. They’re built for different needs:- Enterprise systems like Epic and Cerner are used in big hospitals. They connect to the EHR, lab systems, and billing-all in one place.
- IV compounding systems like Wolters Kluwer’s Simplifi+ are made for hospitals that prepare chemo, antibiotics, or nutrition IVs. They include sterile environment monitoring, dose tracking, and compliance checks for USP <797> and <800> standards.
- Cloud-based workflow tools like Cflow and Kissflow help independent pharmacies manage refill requests, staffing, inventory, and reporting without needing a full hospital-grade system.
Real Results: Numbers Don’t Lie
Studies show these systems cut errors dramatically:- Automated systems detect 14 times more errors than manual checks alone.
- Hospitals using IV compounding automation saw a 70% drop in preparation errors.
- Community pharmacies using barcode verification reduced dispensing errors by up to 85%.
The Hidden Costs: Implementation Isn’t Easy
These systems aren’t plug-and-play. Installing them is like rewiring a house while living in it. Most pharmacies take 3 to 6 months to fully adopt a new system. Staff resist change. Old habits die hard. Training isn’t optional-it’s essential. A pharmacy lead in Adelaide told me: “We had two people quit because they couldn’t learn the new software. We had to hire and train replacements. It hurt.” Costs vary. A small independent pharmacy might pay $15,000 a year for a cloud-based workflow tool. A hospital system with robotics and full EHR integration can spend $200,000 or more annually. And that’s just the license. Add in staff training, IT support, and maintenance. The biggest mistake? Thinking technology fixes everything. It doesn’t. A system is only as good as the people using it. If staff skip scans because they’re rushed, errors come back. If the system is too complex, they find workarounds-and that’s when things break.
What Experts Say About Success
The American Society of Health-System Pharmacists (ASHP) has a simple rule: “Don’t automate a bad process. Fix the process first.” Successful pharmacies don’t just buy software. They redesign their workflow:- They map every step of the old process.
- They identify where errors happen most.
- They involve pharmacists, technicians, and nurses in choosing the system.
- They train everyone-not just once, but repeatedly.
- They measure results: fill times, error rates, patient complaints.
What’s Next: AI, Predictions, and Telepharmacy
The next wave of pharmacy tech isn’t just about automation. It’s about prediction. New systems are starting to use AI to:- Forecast which drugs will run out before they do-based on seasonal trends, prescription patterns, and even weather (flu season spikes demand).
- Flag patients who are likely to miss doses or have adverse reactions before it happens.
- Connect with telehealth platforms so pharmacists can review prescriptions remotely during off-hours.
Final Thought: It’s Not About Tech. It’s About Trust.
Pharmacy workflow systems aren’t magic. They don’t replace judgment. They support it. They give pharmacists the time and tools to do what they were trained for: protect patients. The real win isn’t the barcode scanner or the robot. It’s the mother who no longer has to worry her 80-year-old dad got the wrong blood thinner. It’s the nurse who doesn’t have to double-check a dose because the system already did. It’s the pharmacist who can finally sit down and talk to a patient instead of chasing down a missing label. Technology didn’t save lives. People using technology did.How do pharmacy workflow systems reduce medication errors?
They use automated checks at every step-barcode scanning, drug interaction alerts, dosage validation, and patient identification. These systems catch mistakes before they reach the patient, like wrong doses, allergic reactions, or duplicate prescriptions. Studies show they detect up to 14 times more errors than manual checks alone.
Are pharmacy workflow systems only for hospitals?
No. While hospitals use advanced systems with robotics and IV compounding tools, independent pharmacies use simpler cloud-based platforms like Cflow or Kissflow. These help manage refills, inventory, staffing, and compliance without needing expensive hardware.
What’s the biggest challenge when implementing these systems?
Staff resistance and poor training. Many pharmacies buy the tech but skip redesigning workflows or investing in ongoing education. If pharmacists and technicians don’t understand why the system matters, they’ll find shortcuts-and that’s when errors creep back in.
How much do pharmacy workflow systems cost?
Costs range from $15,000 to $250,000 per year, depending on size and features. Small pharmacies pay less for cloud-based tools. Hospitals with robotics, IV compounding, and full EHR integration pay more. The price includes software, support, training, and updates.
Do these systems comply with safety regulations?
Yes. Leading systems are built to meet USP <797> and <800> standards for sterile compounding, HIPAA for patient privacy, and FDA guidelines for electronic records. They log every action, making audits easier and compliance automatic.
Can AI really help prevent errors in pharmacies?
Yes. New systems use AI to predict drug shortages, flag high-risk patients, and suggest safer alternatives based on a patient’s full history. For example, if a patient is on multiple blood thinners, the system can warn the pharmacist before the script is filled-even if the doctor didn’t see the interaction.


Post A Comment