Food Allergy & Proctitis Symptom Tracker
Track Your Symptoms
Record what you eat and how you feel afterward to identify possible food triggers for your proctitis symptoms.
Your Food Log
Important Note: This tool helps you track patterns but is not a substitute for medical diagnosis. If you experience persistent proctitis symptoms, consult a gastroenterologist for proper evaluation.
Ever wondered why a simple bite of toast can send you running to the bathroom with rectal pain? That uncomfortable combo of symptoms often points to Proctitis, and growing research suggests food allergies might be a hidden trigger.
What Is Proctitis?
Proctitis is inflammation of the rectal lining that can cause bleeding, urgency, tenesmus (a constant feeling of needing to empty the bowels), and abdominal cramping. While infections, radiation therapy, and certain medications are classic culprits, many patients report flare‑ups after meals, hinting at an allergic component.
Understanding Food Allergies
Food allergy is an abnormal immune response triggered by specific proteins in foods, resulting in the release of histamine and other inflammatory mediators. Unlike food intolerance, which is usually a digestive issue, allergy reactions can involve the skin, respiratory system, and, as recent studies show, the lower gastrointestinal tract.
How Food Allergies Can Trigger Proctitis
The link boils down to the body’s immune machinery. When a food allergen crosses the gut barrier, the immune response activates IgE antibodies that bind to mast cells, prompting the release of histamine, prostaglandins, and leukotrienes. Those chemicals increase vascular permeability and attract white blood cells, setting off inflammation that can extend all the way to the rectum.
In addition, chronic exposure to allergens can alter the gut microbiome, reducing protective short‑chain fatty acids and making the rectal mucosa more vulnerable. Researchers at the University of Adelaide (2024) found that patients with allergic rhinitis were three times more likely to develop inflammatory bowel conditions, including proctitis, than non‑allergic controls.
Common Food Triggers
| Allergen | Typical Reaction Time | Key Symptoms (besides proctitis) |
|---|---|---|
| Gluten (wheat, barley, rye) | 30-90 minutes | Bloating, diarrhea, skin rash |
| Dairy (casein, whey) | 15-45 minutes | Gas, abdominal cramp, hives |
| Eggs (ovomucoid) | 10-30 minutes | Nausea, throat itching |
| Tree nuts (almond, walnut) | 20-60 minutes | Swelling, wheezing |
| Shellfish (tropomyosin) | 20-120 minutes | Vomiting, hives |
If you notice a pattern-say, a flare after a cheese pizza-keep a food diary and discuss it with a gastroenterologist.
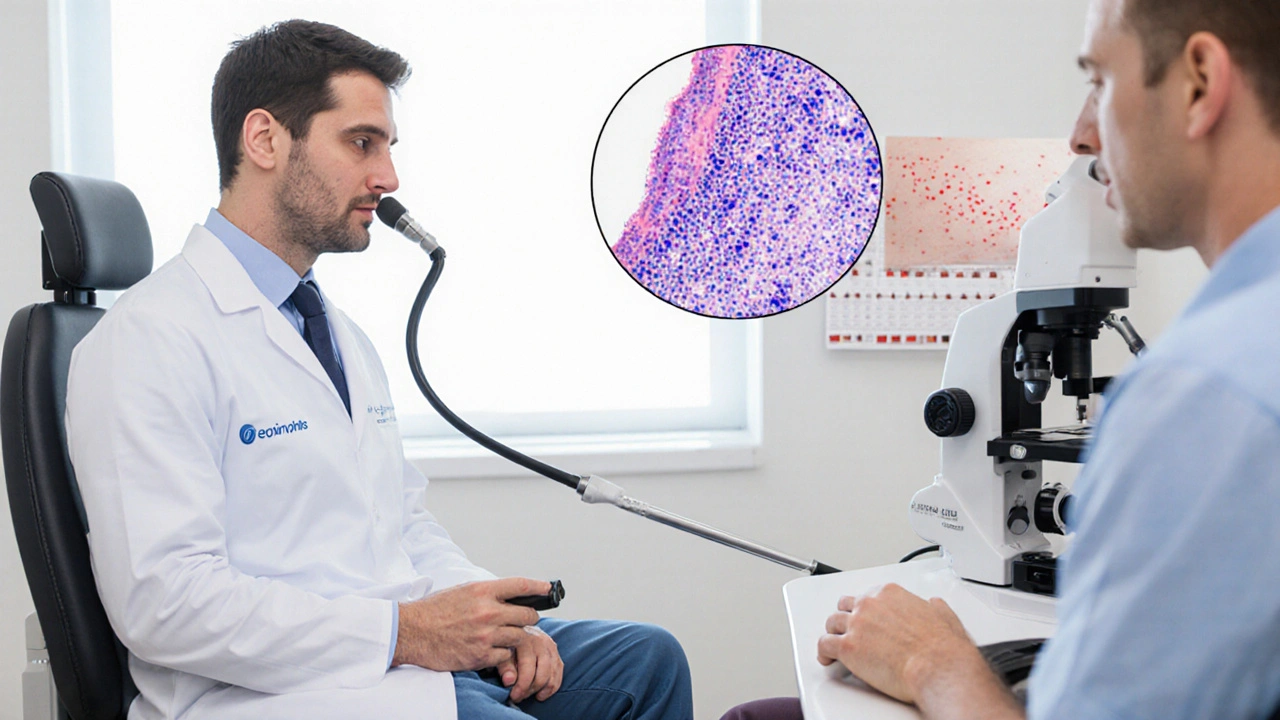
Diagnosing the Connection
Because proctitis symptoms mimic infections and ulcerative colitis, physicians rely on a combination of tests:
- Endoscopy - A flexible sigmoidoscope visualizes the rectal wall. Biopsy samples taken during the procedure are examined for eosinophil infiltration, a sign of allergic inflammation. Biopsy provides microscopic evidence of immune‑mediated damage.
- Allergy testing - Skin prick or serum IgE panels identify specific food sensitivities.
- Elimination diet - Under dietitian supervision, suspected foods are removed for 2-4 weeks. Symptom improvement supports a causal link.
Working with a gastroenterologist a specialist trained in gastrointestinal disorders who can coordinate endoscopic evaluation and dietary management ensures you get an accurate diagnosis.
Managing Proctitis When Food Allergy Is Suspected
- Elimination diet: Remove the top three suspected allergens simultaneously. Re‑introduce one at a time every 7-10 days while monitoring rectal symptoms.
- Medications - Topical 5‑ASA (mesalamine) suppositories reduce local inflammation; short courses of oral steroids may be needed for severe flares.
- Antihistamines - For patients with clear allergic markers, a daily non‑sedating antihistamine can blunt histamine‑driven inflammation.
- Probiotic support - Strains such as *Bifidobacterium longum* and *Lactobacillus rhamnosus* have shown promise in restoring gut barrier function.
- Hydration & fiber - Adequate water and soluble fiber (e.g., oats, psyllium) keep stools soft, reducing mechanical irritation of the inflamed rectum.
If symptoms persist despite diet changes, consider a repeat endoscopy to rule out underlying inflammatory bowel disease.
Lifestyle Tips & Prevention
Even after you identify the trigger, long‑term vigilance helps keep proctitis at bay:
- Keep a digital food‑symptom log; apps like MySymptoms can generate pattern reports for your doctor.
- Read labels carefully-cross‑contamination is common with peanuts and soy.
- Manage stress; cortisol can amplify gut inflammation.
- Schedule annual check‑ups with your gastroenterologist, especially if you have a history of other allergic conditions.
Frequently Asked Questions
Can a food allergy cause bleeding during proctitis?
Yes. Histamine release can increase blood flow and weaken capillary walls in the rectal mucosa, leading to fresh blood on toilet paper or in stool.
Is an elimination diet safe without a dietitian?
Short‑term elimination (2-4 weeks) is generally safe for adults, but you risk missing essential nutrients if you cut out major groups like dairy or wheat. A registered dietitian can ensure balanced nutrition.
How long does it take for symptoms to improve after removing the allergen?
Most patients notice reduced urgency and less bleeding within 3-7 days, though complete mucosal healing may take several weeks.
Do antihistamines replace the need for anti‑inflammatory medication?
Antihistamines target the allergic cascade but don’t directly calm rectal inflammation. Most clinicians use them alongside, not instead of, 5‑ASA or steroids.
When should I see a gastroenterologist versus an allergist?
Start with a gastroenterologist for the proctitis work‑up (endoscopy, biopsy). If they suspect an allergic component, they’ll refer you to an allergist for skin‑prick or IgE testing.



Post A Comment