CCB Interaction Checker
Calculate Your Interaction Risk
Results will appear here after checking your medications
Calcium Channel Blockers: How Metabolic Interactions Affect Drug Clearance and Safety
If you're taking a calcium channel blocker (CCB) for high blood pressure or heart rhythm issues, you might think the medicine is working fine-until you start feeling dizzy, your heart slows down, or your blood pressure drops too low. Often, the problem isn't the drug itself. It's what else you're taking. Calcium channel blockers are among the most commonly prescribed heart medications, but they're also one of the most dangerous when mixed with other drugs. The reason? Their metabolism is tightly controlled by a single enzyme system in your liver, and that system gets easily overwhelmed.
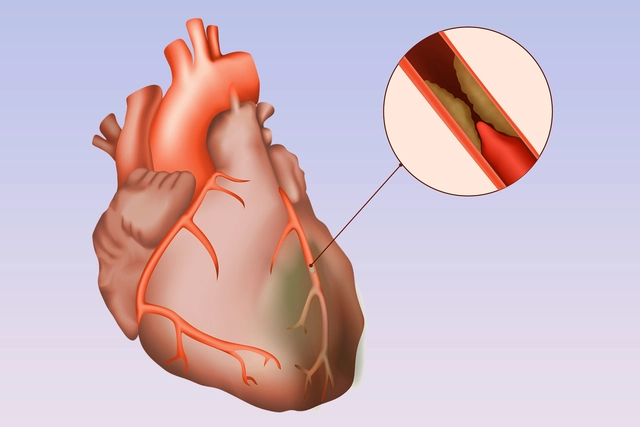
There are two main types of CCBs: dihydropyridines (DHPs) like amlodipine, nifedipine, and felodipine, and non-dihydropyridines (non-DHPs) like verapamil and diltiazem. They both block calcium from entering heart and blood vessel cells, but they do it in different ways. DHPs mainly relax blood vessels, lowering blood pressure. Non-DHPs also slow the heart’s electrical signals, making them useful for arrhythmias. But when it comes to how your body processes them, the differences matter a lot.
How Your Body Breaks Down Calcium Channel Blockers
Almost all CCBs are broken down by an enzyme called CYP3A4. This enzyme lives in your liver and gut and handles about half of all prescription drugs. For DHPs like amlodipine, CYP3A4 does 90% of the work. For verapamil, it’s about 70%. The rest is cleared by the kidneys-but even then, it’s mostly the broken-down pieces, not the original drug. Less than 1% of verapamil or amlodipine leaves your body unchanged in urine.
Here’s the catch: CCBs are also highly bound to proteins in your blood-up to 99% in some cases. That means very little of the drug is floating around freely to do its job. But when something interferes with CYP3A4, the amount of free drug in your blood can spike overnight. Amlodipine’s half-life is 30 to 50 hours, so it builds up slowly. Verapamil, with a half-life of only 4 to 12 hours, gets cleared faster-but when CYP3A4 is blocked, its levels can climb 60-70% higher than normal.
Why Grapefruit Juice Is a Hidden Danger
You’ve probably heard that grapefruit juice can mess with medications. With CCBs, it’s not just a warning-it’s a real risk. Grapefruit contains chemicals that shut down CYP3A4 in your gut. That means more of the drug gets absorbed before it’s broken down. One glass of grapefruit juice can double or even triple the amount of amlodipine or felodipine in your blood. For verapamil, the effect is even stronger.
Patients on CCBs who drink grapefruit juice regularly report dizziness, fainting, and dangerously low blood pressure. One study of over 300 patients found that 68% of those who drank grapefruit juice daily experienced symptoms severe enough to require medical attention. Emergency rooms in the U.S. saw 47 cases in a single year where grapefruit juice combined with a CCB led to collapse or heart rhythm problems. It’s not a myth. It’s a documented pattern.
Other Drugs That Can Turn a Safe CCB Into a Dangerous One
Many common medications also block CYP3A4. These include:
- Antibiotics like clarithromycin and erythromycin
- Fungal treatments like ketoconazole and itraconazole
- HIV drugs like ritonavir and cobicistat
- Antidepressants like fluoxetine and fluvoxamine
- Some cholesterol drugs (statins) like simvastatin and lovastatin
When you take a CCB with one of these, your body can’t clear the CCB fast enough. The result? Toxic levels build up. The FDA has issued 14 safety alerts about CCB interactions since 2020. Nine of them specifically warned about CYP3A4 inhibitors.
Verapamil and diltiazem are especially risky because they don’t just get broken down by CYP3A4-they also block it. That means they can make other drugs stick around longer too. Diltiazem, for example, can raise simvastatin levels by 400%. That’s not just a side effect-it can cause rhabdomyolysis, a condition where muscle breaks down and can lead to kidney failure.
Verapamil also blocks a protein called P-glycoprotein, which normally pumps digoxin (a heart drug) out of your cells. When you take both, digoxin levels can rise by 50-75%. That’s enough to cause dangerous heart rhythms. There are 17 documented cases where this combo caused complete heart block-requiring a pacemaker.
Amlodipine: The Safer Choice for People on Multiple Medications
If you’re on five or more medications, your doctor should consider switching you to amlodipine. Why? Because unlike verapamil and diltiazem, amlodipine doesn’t block CYP3A4. It’s just a substrate-it gets broken down, but it doesn’t interfere with other drugs. Studies show that only 12% of patients on amlodipine need a dose change when taking moderate CYP3A4 inhibitors. For diltiazem, that number jumps to 45%.
Amlodipine also has a long half-life, meaning it stays steady in your system. You take it once a day. There’s less risk of spikes and crashes. It’s also less affected by kidney problems. If your kidneys are weak, you might need to reduce verapamil by half. With amlodipine? No adjustment needed.
Because of this, amlodipine now makes up 42% of all CCB prescriptions in the U.S.-up from 28% in 2020. Doctors are choosing it more often, especially for older patients or those with complex drug regimens.
What Happens When You’re Over 65?
Age changes everything. As you get older, your liver slows down. Your kidneys don’t filter as well. Your body holds onto drugs longer. Patients over 65 are 3.2 times more likely to have severe interactions with CCBs than younger people. And if you have kidney disease-eGFR below 60-you’re 47% more likely to have a bad reaction.
Many elderly patients take statins, blood thinners, diabetes meds, and painkillers-all of which can interact with CCBs. A 2023 report found that 58% of Medicare patients take five or more drugs that can interfere with calcium channel blockers. That’s not rare. That’s normal.
Pharmacists now spend an average of 12.7 minutes per CCB prescription checking for interactions. One in five prescriptions gets flagged and needs a change. That’s why electronic health records now have mandatory alerts. When you prescribe verapamil to someone on clarithromycin, the system pops up: “High risk of bradycardia. Consider switching to amlodipine.”
What You Should Do If You’re Taking a Calcium Channel Blocker
If you’re on a CCB, here’s what you need to know:
- Check your list of medications with your pharmacist. Don’t assume your doctor knows everything you’re taking, including supplements and OTC drugs.
- Avoid grapefruit, Seville oranges, and pomelos. Even small amounts can cause problems.
- If you’re on antibiotics, antifungals, or HIV meds, ask if they interact with your CCB.
- Watch for signs of low blood pressure: dizziness, fainting, fatigue, blurred vision, or a slow heartbeat.
- If you’re over 65 or have kidney problems, ask if amlodipine is a better option.
There’s no need to stop your CCB. But you need to know what’s in your system with it. A simple blood test can check your drug levels if you’re on verapamil or diltiazem with other meds. Not all clinics do this-but if you’ve had side effects, ask for it.
What’s Changing in 2026
The field is moving fast. In March 2023, the FDA approved the first tool called CCB-Check, built into electronic health records. It scans your meds and gives a risk score: green for low, yellow for moderate, red for high. Hospitals using it saw a 31% drop in hospitalizations from CCB interactions.
Researchers are also looking at genetics. About 27% of people have a gene variant that makes CYP3A4 work slower. These people need lower doses of CCBs-even without other drugs. Clinical trials are now testing genetic screening before prescribing CCBs.
And there’s new evidence that your gut bacteria affect how CCBs are broken down. One study found that 34% of the variation in drug clearance could be linked to gut microbiome differences. That means two people on the same dose, with the same liver function, could have totally different drug levels based on what they ate last week.
By 2027, personalized dosing based on metabolism, genetics, and gut health will be standard-not just for CCBs, but for many heart drugs. But for now, the safest approach is simple: know your meds, avoid grapefruit, and ask your doctor if amlodipine might be better for you.
Can I drink grapefruit juice while taking a calcium channel blocker?
No. Grapefruit juice blocks the CYP3A4 enzyme in your gut, which can cause calcium channel blockers like amlodipine, verapamil, or nifedipine to build up to dangerous levels in your blood. This can lead to severe low blood pressure, dizziness, fainting, or even heart rhythm problems. Even one glass can have an effect that lasts over 24 hours. It’s safest to avoid grapefruit, Seville oranges, and pomelos completely while taking any CCB.
Is amlodipine safer than verapamil for people on multiple medications?
Yes. Amlodipine is metabolized by CYP3A4 but does not inhibit it, meaning it’s less likely to interfere with other drugs. Verapamil, on the other hand, blocks CYP3A4 and P-glycoprotein, which can raise levels of statins, digoxin, and many other medications. Studies show only 12% of patients on amlodipine need dose changes when on interacting drugs, compared to 45% for diltiazem and even higher for verapamil. For people on five or more medications, amlodipine is the preferred choice.
What are the signs that a calcium channel blocker is causing a dangerous interaction?
Watch for sudden dizziness, lightheadedness, fainting, unusually slow heartbeat (under 50 bpm), extreme fatigue, blurred vision, or swelling in the legs. These can signal too much drug in your system. If you’re taking a CCB and start a new medication-especially an antibiotic, antifungal, or HIV drug-and feel worse within a few days, contact your doctor immediately. Blood pressure and heart rate should be checked within 24 to 48 hours after starting a new interacting drug.
Do I need blood tests to monitor my calcium channel blocker levels?
Not routinely, but it’s recommended if you’re on verapamil or diltiazem with a CYP3A4 inhibitor, or if you’re elderly, have kidney disease, or are experiencing side effects. Therapeutic levels for verapamil are 50-150 ng/mL. Levels above 200 ng/mL increase the risk of heart block or low blood pressure. Only about 32% of community pharmacies offer this testing, so you may need to ask your cardiologist or pharmacist to arrange it.
Can kidney problems affect how calcium channel blockers work?
Yes. While most CCBs are cleared by the liver, kidney function still matters. If your eGFR is below 60 mL/min, you’re at higher risk for side effects because your body can’t clear metabolites as well. Verapamil requires a 50% dose reduction if your eGFR is between 30 and 60. Amlodipine does not need a dose adjustment for kidney disease. If you have reduced kidney function, ask your doctor if switching to amlodipine is right for you.
What to Do Next
If you’re on a calcium channel blocker, take five minutes today. Pull out your pill bottle and your list of all medications-including vitamins, supplements, and over-the-counter drugs. Look for anything that says “CYP3A4 inhibitor” on the label. Check if you’re drinking grapefruit juice. If you’re over 65 or have kidney issues, ask your doctor if amlodipine is a better fit. Don’t wait for a side effect to happen. These interactions are predictable, preventable, and often overlooked. The right choice can keep you out of the hospital-and keep your heart safe.


Post A Comment