When you pick up a new prescription, you might get a small paper insert with your pills. It looks simple, but this is a Medication Guide-a legally required document designed to tell you exactly what could go wrong and what you need to watch for. These aren’t just paperwork. They’re your personal safety checklist for drugs with serious risks. If you skip reading them, you’re flying blind. And with over 150 guides in use today, knowing how to read them can literally save your life.
Why Medication Guides Exist
The FDA created Medication Guides because some drugs carry dangers that patients need to understand to stay safe. These aren’t for every medication. Only those with risks that can be prevented or reduced if you know what to look for get one. Think blood thinners, antidepressants, cancer drugs, or medicines that can damage your liver or lower your white blood cell count. The goal? Make sure you don’t just take the pill-you know what to do if something goes wrong.
These guides are written at a 6th- to 8th-grade reading level. That means no confusing jargon. They’re supposed to be clear. But many people still miss the point because they don’t know where to look. The real power isn’t in the whole guide-it’s in three specific sections.
Section 1: The Most Important Information
This is the first thing you should read. It’s usually bolded and labeled "What is the most important information I should know about [drug name]?". This section contains the FDA’s most serious warnings-sometimes called "black box" warnings. These aren’t vague. They say exactly what can happen.
For example, the guide for the antidepressant sertraline (Zoloft) says: "Children, teenagers, and young adults may have an increased risk of suicidal thoughts when starting this medicine." That’s not a side effect you can ignore. It’s a red flag that needs attention. The guide for the arthritis drug tofacitinib (Xeljanz) says: "This medicine can increase your risk of serious heart problems, cancer, and blood clots." No sugarcoating. No fluff.
If you see something like this, don’t just skim. Ask yourself: "Does this apply to me?" If you’re under 25 and starting an antidepressant, you need to know the signs of worsening mood. If you have a history of heart disease and are prescribed a drug that raises clot risk, you need to talk to your doctor before taking it.
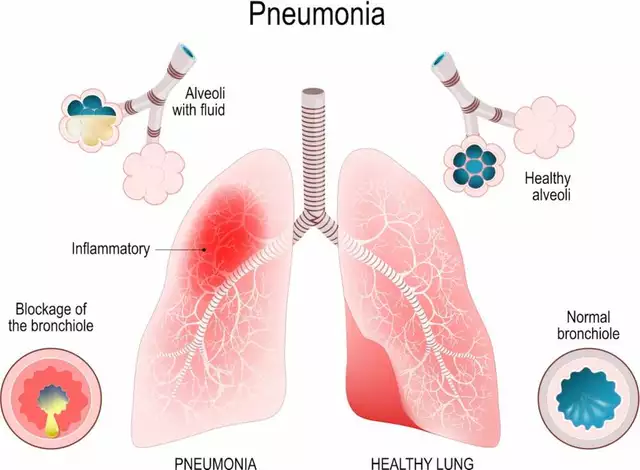
Section 2: Serious Side Effects and Monitoring Instructions
This section tells you what symptoms to watch for-and how often you need to get checked. It’s not enough to know something bad might happen. You need to know how to catch it early.
Look for phrases like:
- "Get your blood tested regularly to check for changes in blood cell counts."
- "Your healthcare provider should perform blood tests before you start and every 3 months while taking this medicine."
- "Call your doctor immediately if you have unusual bruising, bleeding, or fever."
Take warfarin (Coumadin), for example. The guide says you need an INR blood test at least once a month. If your dose changes, you need it more often. That’s not a suggestion-it’s a requirement. Miss a test, and you could bleed internally without knowing it.
Another example: clozapine (Clozaril), used for severe schizophrenia. The guide says, "About 1 in 200 people taking clozapine may develop agranulocytosis," a life-threatening drop in white blood cells. So, you need a blood test every week for the first six months. No exceptions. One missed test could be deadly.
Here’s the trick: cross-reference this section with the next one-"How should I take [drug name]?" That’s where they’ll say things like, "Do not skip your monthly blood test." If both sections say the same thing, that’s your cue: this isn’t optional.

Section 3: Who Should Not Take This Medicine
This part tells you if you’re at higher risk just because of who you are. It’s not about "maybe." It’s about "don’t."
For example:
- "Do not take this medicine if you have severe liver disease."
- "Do not use if you are pregnant or planning to become pregnant."
- "Do not take if you are using certain antibiotics or antifungal medicines."
If you have kidney disease and your new prescription says "avoid if kidney function is below 30%," and you know your GFR is 28%, you need to call your doctor before filling the script. This isn’t a warning-it’s a hard stop.
Many people miss this because they assume their doctor already checked. But doctors are busy. You’re the one who knows your history. If you’ve had a reaction to a similar drug before, or if you’ve had a stroke, or if you’re on another medication-this section is where you connect the dots.
How to Actually Use This Information
Reading the guide isn’t enough. You need to act on it. Here’s how:
- Use the 3-2-1 method: Spend 3 minutes reading it before your first dose. Review it for 2 minutes before each refill. Check for 1 minute every time you take the pill.
- Highlight the red flags: Use a yellow highlighter on any word like "test," "monitor," "check," or "measure." Circle every time frame: "weekly," "monthly," "every 3 months." Underline any symptom that says "call your doctor immediately."
- Create a monitoring calendar: Write down your blood test dates on your phone or a paper calendar. Set reminders. If the guide says "test before starting," schedule it before you even pick up the prescription.
- Use the traffic light system: Green = normal symptoms (mild headache, tiredness). Yellow = warning signs (dizziness, unusual bruising). Red = emergency (chest pain, trouble breathing, black stool). Keep this on your fridge or in your wallet.
- Record it: Keep a simple journal. Write: "Drug: X. Test: Blood count. Due: March 15. Done: Yes/No." Patients who do this have 68% fewer bad reactions.
Pharmacists who use this method say compliance jumps from 45% to 82% when they physically point out the monitoring section and explain it in under 90 seconds. You don’t need to be a doctor. You just need to be paying attention.

What If the Guide Is Missing?
The FDA says you must get a Medication Guide every time you fill a prescription. But a 2022 audit found 41% of independent pharmacies didn’t always give them out. If you don’t get one, ask for it. Say: "I need the Medication Guide for this drug. It’s required by law."
If they say they don’t have it, ask for a digital copy. Go to DailyMed (a free NIH site). Search your drug name. Download the current guide. Print it. Keep it with your pills.
What’s Changing Now?
The FDA is making these guides better. Starting in 2026, they’ll require pictograms-simple icons showing when to test or what symptoms mean. Some drugs already have QR codes that link directly to the latest guide on your phone.
Companies like Pfizer are testing AI tools that pull your medical history and highlight only the risks that apply to you. So instead of reading 10 pages about liver damage, you’d see: "Based on your history of hepatitis B, this drug requires monthly liver tests."
But here’s the hard truth: even with better design, 40% of Americans still struggle to understand medical information. That’s why your action matters. Don’t wait for the system to fix itself. Read the guide. Mark it. Act on it.
What You Should Do Today
Here’s your quick checklist:
- Find your current Medication Guide (ask your pharmacy if you don’t have it).
- Open it to the "Most Important Information" section.
- Read the first two sentences out loud.
- Find the monitoring instructions. Write down the next test date.
- Set a phone reminder for that date.
- Next time you refill, do it again.
It takes less than five minutes. But it might mean the difference between catching a problem early and ending up in the ER.
Are Medication Guides the same as the package insert?
No. Medication Guides are for drugs with serious, preventable risks and are written in plain language for patients. Package inserts are detailed documents meant for healthcare providers, filled with technical terms and dosing charts. You don’t need to read the insert. You absolutely need to read the Medication Guide.
Can I rely on my doctor to explain the risks?
Doctors are under time pressure and often don’t cover everything. A 2021 FDA study found that 60% of patients didn’t recall being told about serious side effects-even when they were listed in the guide. The guide is your backup. Don’t assume your doctor covered it all. Read it yourself.
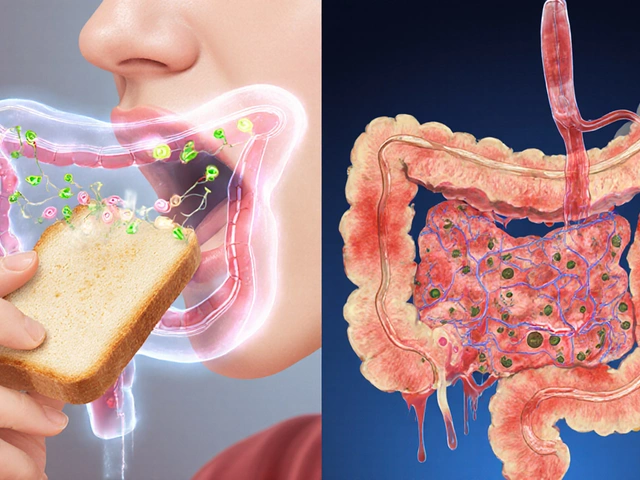
What if I don’t understand a word in the guide?
Look up the term. Use a simple dictionary or search online. For example, if it says "agranulocytosis," type "what is agranulocytosis" into your phone. You’ll find it means a dangerous drop in white blood cells. You can also ask your pharmacist-they’re trained to explain these terms in plain language. No shame in asking.
Do all prescription drugs have Medication Guides?
No. Only about 150 out of thousands of prescription drugs have them. They’re required only for drugs with serious, preventable risks-like blood thinners, certain antidepressants, cancer drugs, and immune system suppressors. If you don’t get one, it doesn’t mean the drug is safe. It just means the FDA doesn’t require a guide for it.
What should I do if I miss a required blood test?
Call your doctor immediately. Don’t wait. If the guide says "test monthly" and you missed two months, your risk may have gone up. Your doctor might need to adjust your dose or stop the drug. Never assume "I’ll get to it next week." For high-risk drugs, missing a test can be dangerous.

Post A Comment