When you see a pill that looks exactly like the brand-name drug you’ve been taking for years-but costs half as much-it’s easy to assume it’s made by a different company. But what if it’s made by the same company that made the brand? That’s not a trick. It’s called an authorized generic, and it’s one of the most common-but least understood-strategies in modern pharmaceuticals.
What Exactly Is an Authorized Generic?
An authorized generic is the exact same drug as the brand-name version, made in the same factory, using the same ingredients, and following the same production process. The only differences? The packaging and the label. No active ingredient changes. No formulation tweaks. No hidden differences. It’s identical in every way that matters to your body. The FDA defines it clearly: an authorized generic is a brand-name drug that’s rebranded and sold as a generic after the patent expires. The manufacturer doesn’t outsource production. They don’t license the formula. They just slap a new label on the same pills they’ve been making for years. This isn’t a loophole-it’s a legal pathway created by the Drug Price Competition and Patent Term Restoration Act of 1984, better known as the Hatch-Waxman Act.Why Would a Brand Company Make Its Own Generic?
It sounds counterintuitive. Why would Pfizer or Eli Lilly give away their own profits? The answer is simple: survival. When a drug’s patent expires, competitors rush in. Within a year, you could have 10 or more generic versions on the market. Prices drop 80-85%. That’s not just a hit-it’s a financial collapse for the brand manufacturer. In 2022, the FDA reported that the average brand-name drug loses over 90% of its revenue within 12 months of generic entry. By launching their own authorized generic, brand companies don’t just survive-they capture a big slice of the new market. Take AstraZeneca’s Prilosec (omeprazole). When the patent expired in 2001, they launched an authorized generic. Within six months, they held 30% of the entire omeprazole market. Competitors got the rest. But AstraZeneca didn’t lose everything. They kept control, kept margins, and kept customers.How Is It Made? The Production Process
There’s no secret factory. No hidden lab. The authorized generic comes from the exact same production line as the brand drug. Here’s how it works:- The company already has FDA approval for the drug’s safety and effectiveness-no new clinical trials needed.
- They file a simple Abbreviated New Drug Application (ANDA) to legally sell it as a generic.
- Manufacturing stays the same: same equipment, same staff, same quality checks.
- They change the packaging: remove the brand name, use plain colors, add the generic label.
- They ship it to distributors under a new brand name-often their own subsidiary.
Market Impact: Who Wins and Who Loses?
The data shows a clear pattern. When a brand company launches an authorized generic:- They capture 15-35% of the generic market in the first year.
- Competing generics see their market share cut in half.
- Prices don’t drop as much as they would without an authorized generic.
Controversy and Criticism
This strategy has drawn sharp criticism. The Federal Trade Commission (FTC) has sued several companies, including Actavis, for using authorized generics to delay real competition. In 2017, Actavis settled for $448 million after the FTC accused them of using an authorized generic to block rivals from entering the market for Namenda. Harvard’s Dr. Aaron Kesselheim argues this isn’t real competition-it’s a way for big pharma to control the market under the guise of lowering prices. His 2022 study in JAMA found that markets with authorized generics saw only a 32% price drop, compared to 68% in markets with only traditional generics. On the other side, PhRMA says authorized generics increase access and maintain quality. The FDA confirms that 99.7% of authorized generics are bioequivalent to their brand counterparts. Patients who switch often report no difference at all.What Do Patients Think?
Patient experiences are mixed. On Drugs.com, authorized generics have a 4.2/5 rating-higher than traditional generics (3.8/5). Comments like “Same pill I’ve been taking for 10 years” are common. But on Reddit, skepticism runs high. One 2023 thread with 147 comments showed 58% of users felt tricked. “Why is my $85 generic only $5 cheaper than the brand? And why does my pharmacist say it’s the same thing?” A 2023 Kaiser Family Foundation survey found 71% of patients preferred authorized generics when available-but 64% didn’t know they were made by the same company. That’s the real issue: transparency.
How Do Companies Plan This?
This isn’t a last-minute move. Companies start planning 2-3 years before a patent expires. They need to:- Set up a separate sales team to avoid mixing brand and generic marketing.
- Redesign packaging to comply with trademark laws.
- Train pharmacists and reps to explain the difference.
- Secure distribution deals with pharmacy chains.
The Future: Biologics and Beyond
Authorized generics started with simple pills. Now they’re moving into complex drugs. In 2023, Amgen launched the first authorized biosimilar-its own version of Enbrel, a biologic drug for autoimmune diseases. This is huge. Biologics are harder to copy. Traditional generics can’t easily replicate them. But the original maker? They already know how. Analysts predict that by 2027, authorized generics will make up 25-30% of the entire generic drug market. That’s up from 18% in 2022. As more expensive drugs lose patents-$250 billion worth between 2023 and 2027-this strategy will only grow.What Should You Do?
If you’re on a brand-name drug that’s about to go generic:- Ask your pharmacist: “Is there an authorized generic?”
- Compare prices: the authorized version might be cheaper than the brand, but not always the cheapest.
- Don’t assume ‘generic’ means ‘different.’ Some generics are made by the same company.
- Check the label: if the manufacturer name matches the brand, it’s likely an authorized generic.
Are authorized generics the same as the brand-name drug?
Yes. Authorized generics are identical to the brand-name drug in active ingredients, strength, dosage form, and how they work in your body. The only differences are the packaging and labeling. They’re made in the same factory, with the same equipment, by the same team.
Why are authorized generics sometimes more expensive than other generics?
Because they’re priced strategically. Brand manufacturers set the price just low enough to keep customers from switching to cheaper generics, but high enough to still make a profit. You might pay $85 for an authorized generic while another version costs $30. The difference comes down to marketing, not quality.
How can I tell if my generic is an authorized generic?
Check the manufacturer name on the bottle. If it’s the same company that makes the brand-name drug-for example, if you’re taking a generic version of Lipitor and the manufacturer is Pfizer-you’re holding an authorized generic. You can also ask your pharmacist directly.
Do authorized generics delay real competition?
Yes, in some cases. The FTC has found that when a brand company launches its own generic, it can block or slow down competitors who are trying to enter the market. This reduces price competition and keeps drug prices higher than they would be otherwise.
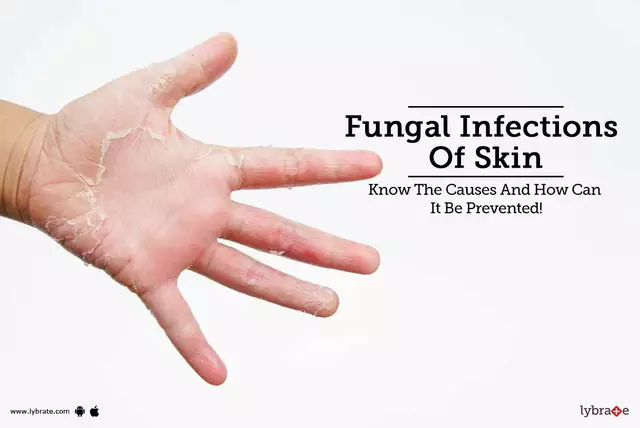
Are authorized generics safe?
Absolutely. Authorized generics are held to the same FDA standards as brand-name drugs. They’re not second-rate. In fact, because they’re made in the same facility with the same process, they’re often more consistent than generics made by third parties.



Post A Comment