Key Takeaways
- Graves' disease spikes metabolism, making it harder to fall asleep and stay asleep.
- Regular sleep‑hygiene habits can blunt the hormone‑driven wake‑up signals.
- Targeted diet tweaks - less caffeine, balanced meals early - help calm nighttime symptoms.
- Medications such as beta‑blockers or antithyroid drugs can improve sleep when symptoms are severe.
- Seek medical advice if insomnia persists longer than four weeks or you notice worsening eye or heart issues.
What Is Graves' Disease?
When it comes to understanding the link between hormones and rest, Graves' disease is an autoimmune disorder that triggers excess production of thyroid hormones, a condition known as hyperthyroidism. The immune system mistakenly attacks the thyroid gland, causing it to grow larger and pump out too much thyroxine (T4) and triiodothyronine (T3). These hormones speed up the body's metabolism, leading to a rapid heart rate, heat intolerance, weight loss, and often a jittery feeling that makes winding down for bed a real challenge.
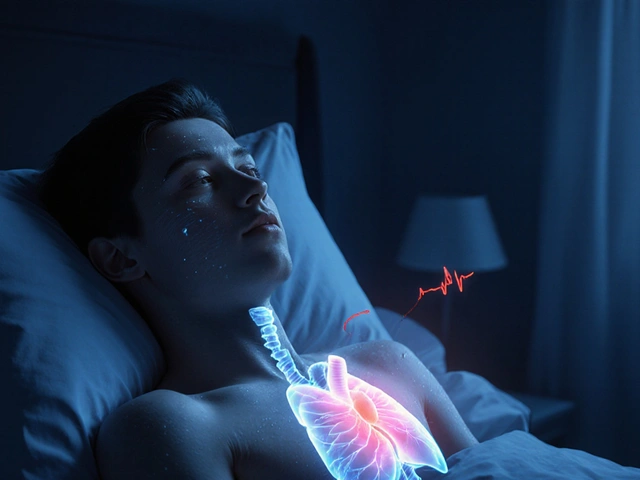
Why Sleep Gets Disrupted
Thyroid hormones act like a revved‑up engine. When levels stay high, the nervous system receives constant “go” signals, which interferes with the brain’s natural transition into the sleep state. Hyperthyroidism creates an over‑active metabolic environment that can raise core body temperature and heart rate at night, both of which are red flags for the body that it’s not time to sleep. Additionally, symptoms such as anxiety, tremors, and night sweats directly feed into insomnia and restless sleep.
Common Sleep Problems Linked to Graves' Disease
- Insomnia difficulty falling or staying asleep - reported by up to 60% of patients in clinical surveys.
- Night sweats - the elevated basal temperature can trigger sudden bursts of heat.
- Frequent awakenings - rapid heartbeats (palpitations) can jolt you awake.
- Restless leg‑type sensations - calcium imbalances from thyroid over‑activity may cause leg twitching.

Non‑Pharmacological Strategies for Better Rest
- Set a consistent bedtime routine. Aim for the same sleep‑and‑wake times even on weekends; the body’s circadian clock loves predictability.
- Dim the lights an hour before bed. Reducing blue‑light exposure lets melatonin rise naturally. Melatonin a hormone that signals darkness to the brain can be supplemented at 0.5mg if you’re over 50, but talk to your doctor first.
- Limit caffeine after 2p.m. Even a small espresso can keep the thyroid‑driven alertness ticking for hours.
- Keep the bedroom cool (around 18°C / 65°F). Lower core temperature encourages the body to enter deep sleep.
- Practice gentle breathing or progressive muscle relaxation for 5‑10 minutes to mute anxiety spikes.
- Schedule meals at least two hours before bedtime; heavy, high‑sugar foods can raise metabolic rate.
Dietary and Supplement Considerations
While there’s no magic diet that cures Graves' disease, certain choices can ease nighttime symptoms:
- Stay hydrated but avoid large fluids right before bed to reduce bathroom trips.
- Eat foods rich in selenium (Brazil nuts, fish) - selenium supports the conversion of T4 to the less active T3, potentially smoothing hormone swings.
- Include complex carbs (whole grains, legumes) early in the evening; they can blunt the adrenaline surge that keeps you awake.
- Watch iodine intake. Excessive iodine (e.g., kelp supplements) may worsen thyroid over‑activity.
When Medication Can Help Your Sleep
If lifestyle tweaks aren’t enough, doctors often turn to the following options:
| Strategy | How It Helps | Typical Use | Considerations |
|---|---|---|---|
| Sleep‑hygiene routine | Regulates circadian rhythm | Daily | Requires consistency; effects build over weeks |
| Melatonin supplement | Boosts nighttime hormone signal | 0.5‑3mg 30min before bed | May cause drowsiness next morning if over‑dosed |
| Beta‑blocker (e.g., propranolol) | Lowers heart rate and tremors, reducing night‑time awakenings | Often taken once daily or as needed | Can cause cold hands, fatigue; contraindicated in asthma |
| Antithyroid medication (methimazole, PTU) | Reduces thyroid hormone production, addressing root cause | Daily dose tailored to labs | Requires regular blood monitoring for liver function |
| Low‑dose trazodone (off‑label) | Sedating effect helps initiate sleep | Taken at bedtime | May cause morning grogginess; not first‑line for thyroid patients |
Only a healthcare professional can decide which medication fits your profile. A typical approach is to first get thyroid hormone levels under control with antithyroid drugs, then add a beta‑blocker if palpitations persist, and finally consider a sleep‑specific agent if insomnia still lingers.

Red Flags: When to Call Your Doctor
- Insomnia lasting longer than four weeks despite lifestyle changes.
- New or worsening eye symptoms (bulging, double vision) - a sign of Graves' ophthalmopathy.
- Chest pain, severe shortness of breath, or irregular heartbeat.
- Sudden weight loss >5% in a month, or persistent trembling that interferes with daily tasks.
Quick Checklist for a Better Night’s Rest
- ✔️ Keep bedtime consistent - aim for 7‑9hours.
- ✔️ Dim lights and shut screens 60minutes before sleep.
- ✔️ Avoid caffeine after 2p.m.; limit alcohol.
- ✔️ Maintain a cool bedroom environment.
- ✔️ Try a low‑dose melatonin if you’re over 50.
- ✔️ Discuss beta‑blocker or antithyroid options with your endocrinologist if symptoms stay high.
Frequently Asked Questions
Can Graves' disease cause nightmares?
Yes. Hormone spikes can increase anxiety and affect REM sleep, which may lead to vivid dreams or nightmares. Managing anxiety and keeping a regular sleep schedule often reduces the frequency.
Is it safe to take melatonin while on antithyroid medication?
Generally, melatonin does not interfere with antithyroid drugs. However, start with a low dose (0.5mg) and monitor for excessive drowsiness. Always check with your doctor before adding any supplement.
Why do I wake up sweating at night?
Elevated thyroid hormones raise basal metabolic rate, increasing body heat. A cooler bedroom and breathable fabrics can help, but persistent night sweats should be discussed with your endocrinologist.
Can beta‑blockers improve my sleep quality?
Beta‑blockers lower heart rate and reduce tremors, which can decrease nighttime awakenings. They don’t act as a sleep aid directly, but many patients report deeper, less fragmented sleep.
Should I avoid exercise before bedtime?
Vigorous exercise within two hours of sleep can raise core temperature and adrenaline, worsening insomnia. Light stretching or yoga earlier in the evening is usually fine.



Post A Comment