More than 95% of people who think they’re allergic to penicillin aren’t. That’s not a guess. It’s what happens when you test them properly. Yet millions of people around the world still avoid penicillin and related antibiotics like amoxicillin because of a label they got as a child - maybe from a rash, maybe from a doctor who didn’t know better. That label sticks. It shows up in every hospital record, every pharmacy system, every doctor’s note. And it’s costing lives, money, and effective treatment.
Why a False Allergy Label Is More Dangerous Than You Think
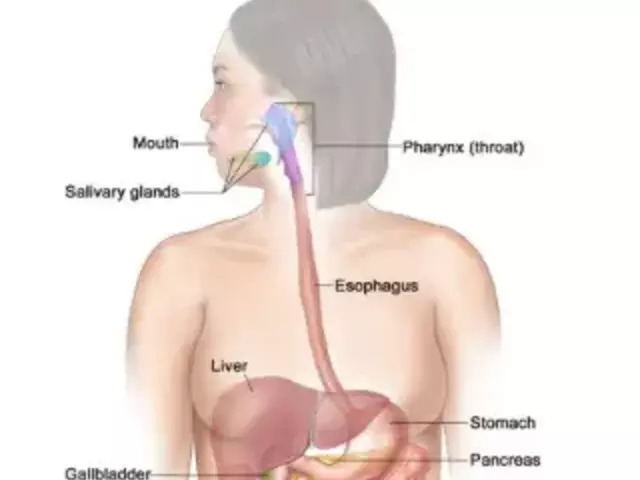
If you’re labeled allergic to penicillin, doctors can’t give you the best, safest, cheapest antibiotic for most infections. Instead, they turn to broader-spectrum drugs like vancomycin, clindamycin, or fluoroquinolones. These drugs aren’t just more expensive - they’re less targeted. They kill good bacteria along with bad ones. That’s why patients with false penicillin allergy labels are 30% more likely to develop Clostridioides difficile infections - a severe, sometimes deadly gut infection caused by antibiotic overuse. The CDC estimates that false penicillin labels lead to 50,000 extra C. diff cases every year in the U.S. alone. That’s not just a number. It’s people who end up in the hospital for weeks, with diarrhea, fever, and complications that could have been avoided. And it’s not just C. diff. These broader antibiotics are fueling antibiotic resistance. Patients with a penicillin label are nearly 70% more likely to get clindamycin, which has pushed up MRSA rates. They’re 28% more likely to get fluoroquinolones, linked to rising E. coli resistance. And the cost? On average, each patient with a false label adds $1,000 to their annual healthcare bill. Multiply that by millions of people. That’s billions of dollars wasted every year on drugs that aren’t needed, longer hospital stays, and preventable complications.What’s Really Going On? The Truth About Penicillin Allergies
Most people don’t actually have a true IgE-mediated penicillin allergy. That’s the kind that causes hives, swelling, trouble breathing, or anaphylaxis - the scary stuff. But many labels come from rashes, nausea, or headaches - side effects that aren’t allergies at all. In fact, studies show that 75% of all drug allergy labels are wrong. Even more surprising: if you were told you were allergic to penicillin 20 years ago, there’s a 90% chance you’re no longer allergic. Allergies can fade over time. The immune system forgets. But your record doesn’t. That’s why testing isn’t just helpful - it’s necessary.How Do You Know If You’re Really Allergic?
There are three main ways to find out if your allergy label is real:- Skin testing - A small amount of penicillin is placed under your skin. If you’re allergic, you’ll get a red, itchy bump within 15-20 minutes. This test is highly accurate for immediate reactions.
- Drug provocation test - You take a small, increasing dose of penicillin (like amoxicillin) under medical supervision. If you don’t react, the label is removed. This is the gold standard for non-immediate reactions.
- Combined approach - Skin test first, then oral challenge if the skin test is negative. This is the most reliable method, with a 98% negative predictive value. If both are negative, you’re almost certainly not allergic.

Who Can Do This Testing? You Don’t Need an Allergist
You might think you need to see an allergy specialist. You don’t. More and more hospitals and clinics are training primary care doctors, pharmacists, and nurses to do this safely. A 2021 study showed that after just 10 supervised cases, non-allergists were following guidelines correctly 92% of the time. Tools like the PEN-FAST score help doctors decide who’s low-risk. It’s a simple five-question checklist:- Was your reaction 5 or more years ago?
- Was it just a rash?
- Did you have no other symptoms like swelling or breathing trouble?
- Did you not need treatment for it?
- Did you take penicillin again since then without a problem?
What Happens After the Test?
If you pass, your allergy label is removed. But it doesn’t just disappear from your chart. It gets updated - specifically. Instead of “Penicillin Allergy,” it becomes “Penicillin Allergy - Ruled Out.” Some systems even write “Tolerated amoxicillin on [date].” This matters because not all penicillins are the same. Amoxicillin and ampicillin are closely related. But some other antibiotics, like cephalosporins, have very low cross-reactivity. A broad label can block you from safe, effective drugs you could have taken. And here’s the kicker: once you’re de-labeled, you’re more likely to get the right antibiotic next time. That means faster recovery, fewer side effects, and less risk of antibiotic resistance.Real Stories: What Patients Say
One patient from Mayo Clinic had been told she was allergic to penicillin since age 5. She got a rash once. That was it. For 20 years, she avoided penicillin. Every time she got a sinus infection, she got azithromycin - a Z-Pak. It always gave her nausea and diarrhea. After testing, she found out she wasn’t allergic. She took amoxicillin for her next infection. No side effects. No fuss. She said it felt like a weight had been lifted. Another patient in Australia had a false label for 40 years. He kept getting urinary tract infections because doctors wouldn’t give him the best antibiotic. He ended up in the hospital twice. After testing and de-labeling, he was able to take amoxicillin again. His infections cleared faster. He saved over $28,000 in hospital costs over two years. But not everyone has a smooth experience. One Reddit user had a direct challenge without skin testing - and got mild wheezing. He was correctly labeled allergic afterward, but he wished they’d done skin testing first. That’s why proper risk assessment matters.
Why Isn’t Everyone Getting Tested?
You’d think this would be standard by now. But it’s not. Only about 12% of U.S. hospitals have full de-labeling programs built into their systems. Why?- Wait times - You might wait 14 weeks just to get an appointment.
- Lack of awareness - Many doctors still don’t know how to do it or think it’s too risky.
- Electronic health records - Some systems don’t let you easily remove or update allergy labels.
- Patient fear - People are scared to try again. They’ve lived with the label for decades.
What You Can Do Today
If you’ve been told you’re allergic to penicillin:- Check your medical records. What exactly was the reaction? Was it a rash? Nausea? Or something serious?
- Ask your doctor: “Could I have been mislabeled? Is testing an option?”
- Ask about PEN-FAST. If you scored low, you may be a candidate for a simple oral challenge.
- Don’t assume you’re allergic forever. Allergies fade.
- If your hospital doesn’t offer testing, ask if they can refer you to a clinic that does.
Final Thought: A Label Shouldn’t Limit Your Care
A penicillin allergy label isn’t a life sentence. It’s a mistake waiting to be corrected. And correcting it isn’t just science - it’s common sense. If you’re avoiding a safe, effective, cheap antibiotic because of something that happened 30 years ago, you’re not being cautious. You’re being misled. Testing is safe. It’s fast. It’s affordable. And it gives you back control over your own health.Can I outgrow a penicillin allergy?
Yes. Most people who had a penicillin allergy as a child lose it over time. Studies show that 80% of people who were allergic 10 years ago are no longer allergic by 20 years later. The immune system can forget the reaction. That’s why testing is important - even if you’ve avoided penicillin for decades.
Is skin testing painful?
Skin testing feels like a tiny pinch - similar to a blood test. It’s not painful. The most common side effect is mild redness or itching at the test site, which goes away in an hour or two. Serious reactions during skin testing are extremely rare.
What if I react during the test?
If you have a reaction during testing, the medical team stops immediately and treats it. Reactions are almost always mild - like a rash or stomach upset. Severe reactions like anaphylaxis are rare, especially in low-risk patients. Testing is done in a controlled setting with emergency equipment on hand.
Will my insurance cover this?
Most insurance plans, including Medicare and Medicaid, cover drug allergy testing when it’s medically necessary. Many hospitals now include it as part of antibiotic stewardship programs, so there’s often no extra cost to you. Always check with your provider, but don’t assume it’s too expensive - the cost of avoiding penicillin is far higher.
Can I test for other antibiotics besides penicillin?
Yes. While penicillin is the most common, testing is also available for other antibiotics like cephalosporins, sulfa drugs, and vancomycin - especially if you’ve had a reaction. However, testing protocols vary by drug. Penicillin is the most studied and easiest to test for.
How long does the whole process take?
It depends on your risk level. Low-risk patients can complete a direct oral challenge in under 2 hours - one dose, then observation. Skin testing plus challenge usually takes 2-3 hours total. Most people are done in a single visit. You won’t need to come back multiple times.
Will I be able to take amoxicillin after testing?
If your test is negative, yes. Amoxicillin is the most commonly prescribed penicillin-type antibiotic. It’s safe, effective, and often the first choice for ear, sinus, and urinary tract infections. After de-labeling, you can take it without fear - and avoid the side effects of broader antibiotics.




Post A Comment