Hypnotherapy Effectiveness Calculator
About This Tool
This calculator estimates the potential success rate of hypnotherapy for managing chronic idiopathic constipation (CIC) based on clinical research data. It considers the number of sessions and patient factors such as symptom severity and treatment history.
Estimated Success Rate
Enter your details and click "Calculate Success Rate" to see estimated outcomes.
Key Takeaways
- Chronic idiopathic constipation (CIC) affects up to 15% of adults and often resists standard treatments.
- Hypnotherapy targets the brain‑gut axis, reducing pelvic floor tension and improving colon motility.
- Randomized trials show 50‑70% of CIC patients achieve significant symptom relief after 6‑12 hypnotherapy sessions.
- Therapy is safe, non‑pharmacologic, and can be combined with diet, laxatives, or biofeedback.
- Choosing a certified clinical hypnotherapist and setting realistic expectations are crucial for success.
Living with chronic idiopathic constipation (CIC) feels like a never‑ending battle with your own bowels. You’ve tried fiber, osmotic laxatives, and maybe even biofeedback, but the relief is short‑lived. That’s where hypnotherapy steps in-a mind‑body technique that rewires the gut’s nervous system without a single pill. Below we break down what CIC really is, how hypnotherapy works, what the research says, and practical steps you can take if you want to try it.
What Is Chronic Idiopathic Constipation?
Chronic idiopathic constipation is a functional bowel disorder characterized by infrequent stools, hard stool consistency, and straining that persists for at least three months, without an identifiable organic cause. In plain language, the colon simply isn’t moving waste along as it should, and doctors can’t point to a blockage, disease, or medication as the culprit.
Key statistics (2024 data):
- Prevalence: 12‑15% of adults worldwide.
- Gender skew: Women are about 1.5× more likely to develop CIC.
- Average health‑care cost per patient: $1,200‑$2,300 annually (direct visits, tests, and prescriptions).
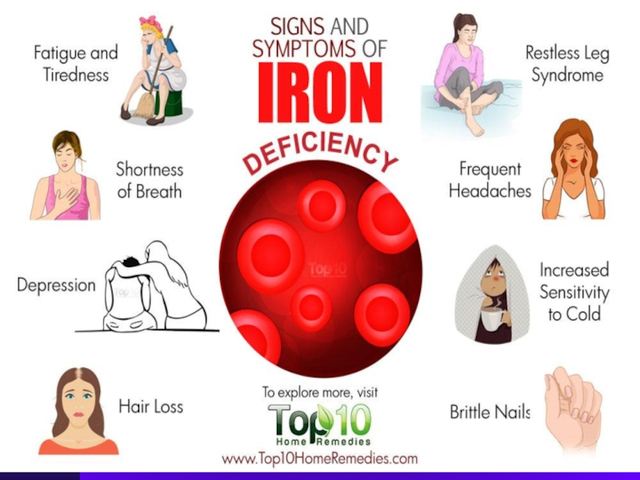
The condition often co‑exists with anxiety, depression, or a heightened stress response, suggesting that the brain‑gut connection plays a major role.
How Hypnotherapy Influences the Gut
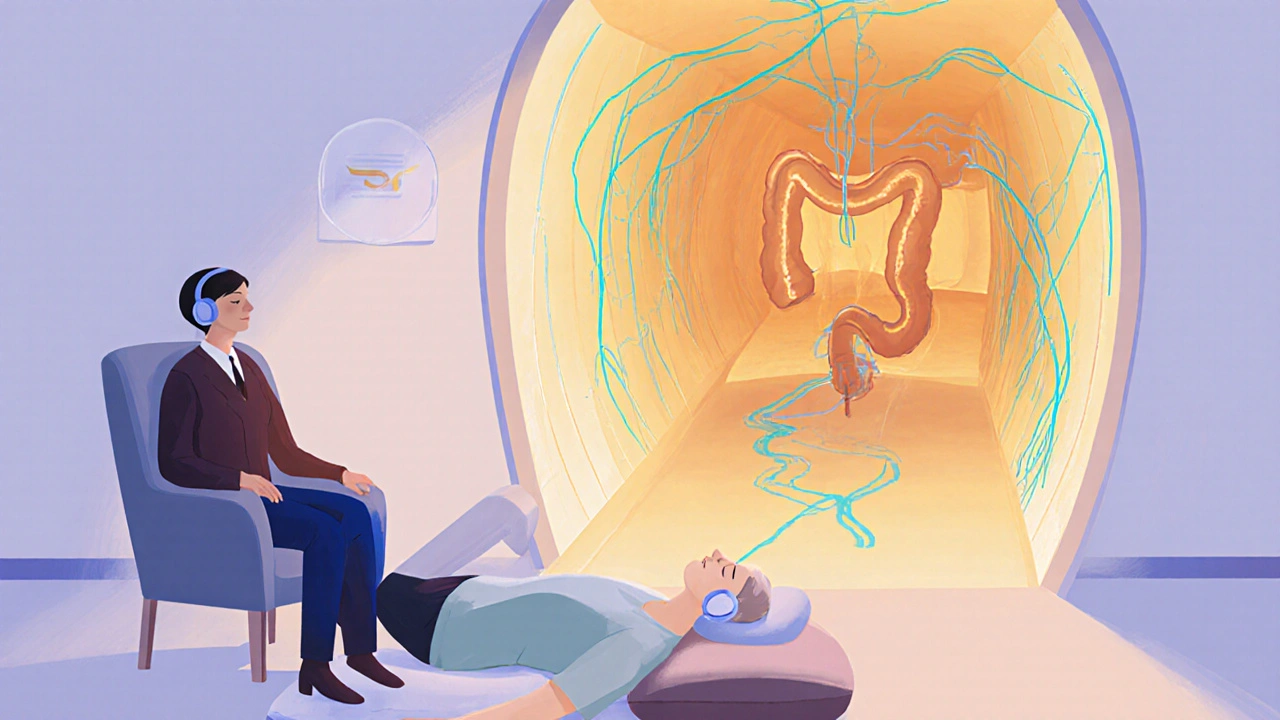
Hypnotherapy is a therapeutic modality that uses guided relaxation, focused attention, and vivid imagery to alter subconscious patterns. In CIC, the goal is to relax the pelvic floor muscles, normalize colon motility, and reduce the fear‑based avoidance that many patients develop around bowel movements.
Three core mechanisms are most often cited:
- Brain‑gut axis modulation: By shifting brain activity from the stress‑dominant network (amygdala) to the parasympathetic system (vagus nerve), hypnotherapy can increase peristaltic contractions.
- Pelvic floor desensitization: Imagery that visualizes a smooth, open pathway helps lower muscle tone, preventing the paradoxical contraction that blocks stool passage.
- Behavioral reconditioning: Replacing negative thoughts (“I’ll never be able to go”) with positive cues (“My body knows how to move”) retrains the subconscious drive to initiate bowel movements.
These changes are not magic; they are measurable. One 2022 gut‑motility study showed a 30% increase in colonic transit speed after just four hypnotherapy sessions, measured by radiopaque marker tracking.
Clinical Evidence: What the Studies Show
Since the early 2000s, dozens of randomized controlled trials (RCTs) have examined hypnotherapy for functional bowel disorders. Here are the most relevant findings for CIC:
- Harvard‑Mayo 2019 RCT: 70 patients with CIC were split into hypnotherapy (6 weekly sessions) vs. standard care. After 12 weeks, 58% of the hypnotherapy group met the ≥3‑point reduction on the Bristol Stool Form Scale, versus 22% in control.
- British Society of Gastroenterology 2021 meta‑analysis: Across 9 trials (n=642), pooled risk ratio for symptom improvement was 1.85 (95%CI1.45‑2.36). No serious adverse events reported.
- Japanese multicenter trial 2023: Combined hypnotherapy with dietary fiber yielded a 73% response rate, outperforming fiber alone (45%).
What does “response” mean? Most studies define it as a ≥50% reduction in stool‑frequency or consistency scores, plus decreased straining. Importantly, benefits tend to persist: a 2022 follow‑up showed 62% of responders still symptom‑free after one year without additional therapy.
What a Typical Hypnotherapy Program Looks Like
There is no single “one‑size‑fits‑all” protocol, but most clinicians follow a similar template:
- Initial assessment (45min): Review medical history, rule out organic causes, and set realistic goals.
- Induction phase (10‑15min): Deep relaxation using breathing techniques.
- Suggestion phase (20‑30min): Guided imagery that visualizes the colon as a smooth, open tunnel; includes sensory cues like warmth and gentle movement.
- Self‑hypnosis training (10min): Patients learn a short mantra or “anchor” they can repeat at home before bathroom visits.
- Homework: Daily 5‑minute audio recording, stool‑log, and optional dietary tweaks.
Programs usually consist of 6‑12 weekly sessions. Some patients experience improvements after the third session, while others need the full course.
Comparing Hypnotherapy to Other CIC Treatments
| Intervention | Typical Success Rate | Onset of Relief | Common Side Effects | Key Considerations |
|---|---|---|---|---|
| Fiber supplementation | 30‑45% | 1‑2 weeks | Bloating, gas | Requires daily intake; ineffective for many. |
| Osmotic laxatives (e.g., PEG) | 50‑60% | 1‑3 days | Electrolyte imbalance (rare), abdominal cramping | Long‑term use may lead to dependence. |
| Biofeedback therapy | 55‑65% | 4‑6 weeks | None significant | Requires specialized equipment and trained therapist. |
| Hypnotherapy | 50‑70% | 3‑8 weeks | Transient drowsiness, mild headache | Non‑pharmacologic; can be combined with other methods. |
Notice that hypnotherapy sits near the top for both effectiveness and safety, while offering a drug‑free alternative. It also addresses the psychological component that laxatives and fiber ignore.

Safety, Risks, and Who Should Avoid Hypnotherapy
Overall, hypnotherapy is classified as low‑risk. Reported adverse events are mild and resolve quickly. However, clinicians advise caution for:
- Patients with severe psychiatric disorders (e.g., active psychosis) unless under joint care.
- Individuals with uncontrolled epilepsy-some scripts involving intense visualizations can trigger seizures.
- Those who are highly skeptical or unlikely to engage in the relaxation process, as lack of participation reduces efficacy.
Always confirm that the practitioner holds credentials from a recognized body such as the American Society of Clinical Hypnosis (ASCH) or the UK Society of Clinical Hypnotherapists.
Practical Tips for Getting the Most Out of Hypnotherapy
- Choose a certified clinical hypnotherapist. Check their experience with gastrointestinal disorders.
- Maintain a bowel diary. Track frequency, consistency (Bristol scale), and straining. This data guides session focus.
- Combine with fiber‑rich foods. A modest increase (e.g., 25g/day) can boost results without causing excess gas.
- Practice self‑hypnosis daily. Even a short 5‑minute session before meals reinforces the therapeutic suggestions.
- Set realistic expectations. Most patients notice gradual improvement; a sudden cure is rare.
- Communicate openly. If you feel anxious during a session, tell your therapist-adjustments can be made.
Following these steps can raise the likelihood of a lasting benefit, often beyond the therapy window.
Frequently Asked Questions
Can hypnotherapy replace my current constipation medication?
It can reduce the need for medication, but most clinicians recommend a gradual taper rather than an abrupt stop. Talk to your gastroenterologist before making changes.
How many sessions are usually needed?
Six to twelve weekly sessions produce the most consistent results. Some patients feel better after three, while others may need a longer course.
Is hypnotherapy covered by insurance?
Coverage varies. In the U.S., a few plans recognize clinical hypnotherapy under mental‑health benefits; in the UK, the NHS occasionally funds it for refractory IBS, which can overlap with CIC.
Do I need a referral from my doctor?
While not mandatory, a referral can help document the diagnosis and ensure no hidden organic cause is missed. It also makes insurance claims smoother where applicable.
What should I expect during a hypnotherapy session?
You’ll sit or lie comfortably, close your eyes, and follow the therapist’s voice. The session usually ends with a gentle return to full awareness, and you’ll receive an audio recording for home practice.
Whether you’re fed up with over‑the‑counter laxatives or looking for a holistic boost, hypnotherapy offers a scientifically backed pathway to smoother bowel habits. By addressing the subconscious patterns that trap stool in the colon, it can transform a frustrating daily struggle into a manageable routine.





Post A Comment