Most people assume that a generic pill is just as good as the brand-name version. After all, the FDA says they’re the same. But if you’ve ever switched from Synthroid to a generic levothyroxine and suddenly felt exhausted, moody, or off-balance, you’re not alone. And you’re not imagining it. For some medications, especially those with a narrow therapeutic index, even tiny differences in how the body absorbs the drug can lead to real, measurable changes in how you feel - or even put you at risk.
What Does ‘Bioequivalent’ Really Mean?
When the FDA approves a generic drug, it doesn’t require new clinical trials. Instead, it checks if the generic delivers the same active ingredient at roughly the same speed and amount as the brand. The rule? The generic must deliver between 80% and 125% of the brand’s blood concentration. That’s a huge range. Two generics made by different companies could be 45% apart in how much of the drug gets into your bloodstream - and both could still be labeled ‘bioequivalent.’Think of it like two different brands of coffee. Both have caffeine. One brews strong, one brews weak. The FDA says if they’re both between 80% and 125% of the original’s strength, they’re the same. But if you’re sensitive to caffeine, that 20% difference might keep you up all night. For some drugs, that kind of variation isn’t just inconvenient - it’s dangerous.
When Small Differences Become Big Problems
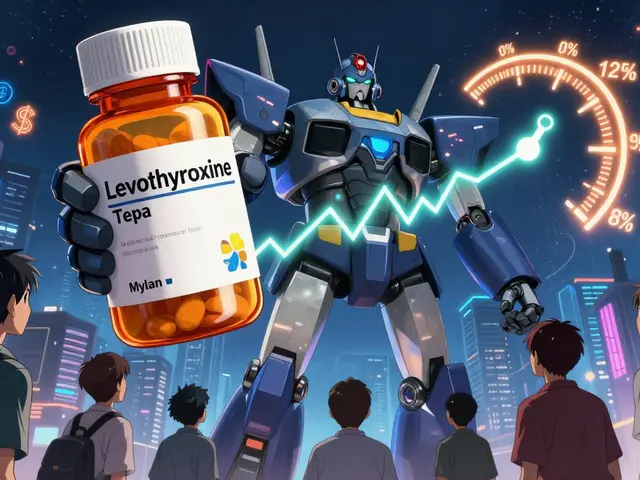
Not all drugs are created equal. Medications with a narrow therapeutic index (NTI) have a razor-thin margin between helping you and hurting you. A little too much, and you overdose. A little too little, and the treatment fails. These include:- Levothyroxine (for hypothyroidism)
- Warfarin (a blood thinner)
- Phenytoin and carbamazepine (for seizures)
- Digoxin (for heart rhythm)
A 2019 study in JAMA Internal Medicine followed over 2,000 people who switched from brand-name Synthroid to generic levothyroxine. Nearly 24% had thyroid hormone levels swing out of the safe range within six months. That’s more than one in four. People who stayed on the brand? Only 14% had the same issue.
For patients on warfarin, a blood thinner used after heart attacks or for atrial fibrillation, even a 10% change in drug levels can trigger dangerous clots or bleeding. The American College of Chest Physicians recommends checking INR levels - a blood test that measures clotting time - just 3 to 5 days after switching generics. Many doctors don’t even know this is necessary.
It’s Not Just the Active Ingredient
The active ingredient in a generic is identical to the brand. But that’s only 1% to 20% of the pill. The rest? Fillers, dyes, binders, coatings - things called excipients. These don’t treat your condition. But they can affect how your body absorbs the drug.Some generics use different coatings that dissolve slower or faster. Others use preservatives like bisulfites, which can trigger asthma attacks in 5-10% of asthmatic patients. A patient with asthma might switch from one generic to another and suddenly struggle to breathe - not because the medicine changed, but because the filler did.
One patient on Reddit described switching from one generic bupropion (used for depression and smoking cessation) to another and getting severe headaches within hours. Another said they felt ‘like a different person’ - anxious, jittery, unable to sleep. These aren’t rare anecdotes. A 2023 survey of over 1,200 patient reviews on Drugs.com showed 38% of people on generic levothyroxine felt their symptoms worsened compared to the brand. Twenty-eight percent reported increased fatigue. Nearly 20% said their mood changed.
What the Data Doesn’t Tell You
The FDA says 99.7% of generics meet bioequivalence standards. That’s true. But that number doesn’t tell you how many people feel worse after switching. It doesn’t capture the patient who had to go back to the brand because they couldn’t work, couldn’t sleep, or kept having seizures. It doesn’t reflect the pharmacist who sees five patients a month come in confused because their ‘same’ medication suddenly made them sick.A 2022 survey of 3,215 community pharmacists found that 68% had seen patients react badly after switching between different generic versions of the same drug. Over 40% said this happened frequently - more than five cases a month. And yet, most patients aren’t warned. Pharmacists are often required by law to substitute generics unless the doctor specifically says ‘dispense as written.’
Some doctors assume all generics are interchangeable. But the FDA itself gives 4% of generic drugs a ‘BX’ rating - meaning they might not work the same for everyone. These are the ones you should ask about.
Who’s Most at Risk?
It’s not just about the drug. It’s about the person.- People with chronic conditions - like thyroid disease or epilepsy - rely on rock-solid consistency. A tiny change can undo months of stabilization.
- Older adults often take multiple medications. Switching one generic can throw off the whole system.
- People with allergies or sensitivities might react to a dye or preservative that wasn’t in their previous version.
- Patients on complex regimens - like those with HIV, heart failure, or organ transplants - are especially vulnerable. A 2019 study showed 28% of these patients had adverse effects when switching between generic manufacturers.
One woman in Adelaide told me she’d been stable on Synthroid for eight years. After a pharmacy switch, her doctor didn’t check her TSH for three months. By then, her heart was racing, her weight had dropped 12 pounds, and she couldn’t concentrate at work. It took two more blood tests and a switch back to the brand to fix it.
What You Can Do
You don’t have to accept unpredictable side effects. Here’s what works:- Ask your doctor to write ‘dispense as written’ on prescriptions for NTI drugs. This prevents automatic substitution.
- Check the pill’s appearance - color, shape, imprint. If it looks different, ask your pharmacist why. It might be a different generic.
- Keep a symptom diary - note energy levels, mood, sleep, heart rate, or seizures after any switch. This helps your doctor spot patterns.
- Use the FDA’s Inactive Ingredient Database - if you know you’re allergic to certain dyes or preservatives, look up the generic’s ingredients before accepting it.
- Request the authorized generic - in 2023, the FDA approved an authorized generic version of Synthroid. It’s made by the same company as the brand, with the exact same ingredients. It’s cheaper than the brand but just as consistent.
Why This Matters Beyond the Pill
Generic drugs save the U.S. healthcare system over $370 billion a year. That’s huge. But if we’re trading savings for more hospital visits, more ER trips, or more failed treatments, we’re not really saving anything.Research from the Bipartisan Policy Center suggests that if we made manufacturing standards stricter for NTI drugs - like the EU already does - we could prevent 142,000 adverse events every year. The cost? Maybe a 5% increase in generic prices. That’s less than the cost of one missed workweek for most people.
The truth is, not all generics are equal. And not everyone reacts the same way. For most drugs - like metformin for diabetes or statins for cholesterol - switching generics is fine. But for the few that matter most to your daily life, consistency isn’t a luxury. It’s a necessity.
If you’ve ever felt ‘off’ after a pharmacy switch - even if your doctor says it’s ‘just in your head’ - trust yourself. Your body knows the difference. And you deserve a medication that works, every time.
Can generic medications really be different from brand-name ones?
Yes. While the active ingredient must be identical, the inactive ingredients - like fillers, dyes, and coatings - can vary between brands and generics. These differences can affect how quickly or completely your body absorbs the drug, especially for medications with a narrow therapeutic index like levothyroxine or warfarin.
Which generic drugs are most likely to cause problems?
Drugs with a narrow therapeutic index (NTI) are the highest risk. These include levothyroxine (for thyroid), warfarin (blood thinner), phenytoin and carbamazepine (anti-seizure), and digoxin (heart medication). Even small changes in blood levels can lead to serious side effects or treatment failure.
How do I know if I’m reacting to a generic drug?
Watch for changes in symptoms after switching: increased fatigue, mood swings, headaches, seizures, heart palpitations, or unexplained weight changes. Keep a diary of when you switched and what happened. If symptoms appear shortly after a pharmacy change, talk to your doctor - it might not be coincidence.
Should I avoid all generic medications?
No. For most medications - like metformin, lisinopril, or atorvastatin - generics work just as well. The issue is limited to a small group of drugs where consistency is critical. Ask your doctor or pharmacist if your medication is on the NTI list. If not, generics are usually safe and cost-effective.
Can I request the brand-name drug instead of a generic?
Yes. Your doctor can write ‘dispense as written’ or ‘no substitution’ on your prescription. You can also ask for the authorized generic - made by the original brand’s company - which has the same ingredients but costs less than the brand-name version.
Why don’t pharmacists warn me about possible side effects from switching generics?
In many places, pharmacists are legally required to substitute generics unless the doctor says otherwise. Many aren’t trained to recognize subtle differences in patient response, and the system prioritizes cost savings over individual variation. It’s up to you to speak up if you feel something’s off.
Are there any tests to predict how I’ll react to a generic?
Yes. Pharmacogenomic testing - which looks at how your genes affect drug metabolism - can predict your response to certain medications with up to 84% accuracy. While not yet routine, it’s becoming more accessible and may soon help guide which generic, if any, is safest for you.
What Comes Next?
If you’re on a medication with a narrow therapeutic index, don’t wait for a crisis. Talk to your doctor about your history with generics. Ask if your drug is on the FDA’s list of high-risk NTI medications. Request a blood test after any switch - even if you feel fine. Keep a log. Be your own advocate.The system is built to save money. But your health shouldn’t be the cost.





Post A Comment