Decision-Making Errors: Why Smart Choices Go Wrong and How to Fix Them
When it comes to health, decision-making errors, mistakes in choosing, trusting, or following medical advice that lead to harm. Also known as clinical judgment failures, these aren’t just about forgetting a pill—they’re about misreading risk, misunderstanding labels, or trusting something that looks right but isn’t. You might think you’re being careful, but small oversights—like accepting a cheap generic without checking the pharmacy, or assuming a penicillin allergy label is final—can have serious consequences. These errors don’t happen because people are careless. They happen because the system is confusing, the information is hidden, and the stakes are high.
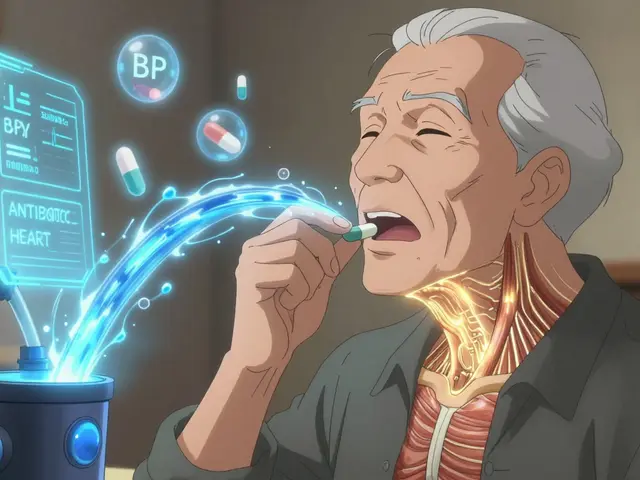
Take false drug allergy, when someone is wrongly labeled allergic to a common medication like penicillin. Also known as drug allergy de-labeling, it affects over 95% of people who think they’re allergic. That label sticks for decades, even though testing proves it’s wrong. The result? Doctors give less effective, more expensive, or riskier antibiotics. That’s a decision-making error rooted in outdated assumptions. Or consider counterfeit meds, fake pills that look identical to real ones but contain toxic substances like fentanyl or chalk. Also known as fake prescription pills, they’re sold online as cheap alternatives. People make the mistake of trusting a low price over a trusted pharmacy. The body reacts, but the cause? A decision made without verifying the source.
Even something as simple as tracking your meds can go wrong. medication adherence, how consistently a patient takes their prescribed drugs. Also known as pill tracking, it’s one of the biggest hidden problems in healthcare. Paper logs fail. Memory fades. People skip doses because they’re confused, overwhelmed, or afraid of side effects. That’s not laziness—it’s a system failure. And when patients don’t stick to their plan, doctors assume the drug isn’t working. So they change it. Or add another. And another. More pills. More cost. More risk. All because the first decision—tracking adherence—wasn’t supported properly.
Behind every bad decision is a missing piece: oversight. quality assurance units, independent teams that check drug safety before it reaches patients. Also known as GMP compliance teams, they’re the last line of defense. When these units aren’t truly separate from production, mistakes slip through. A batch of pills passes testing because the same people who made them also checked them. No one’s watching. No one’s asking hard questions. That’s how contaminated meds, wrong dosages, or ineffective generics end up on shelves. It’s not a glitch. It’s a structural flaw.
These aren’t abstract problems. They show up in real stories: a child’s growth delay because celiac disease was missed, a kidney transplant patient getting sick because they skipped a vaccine, someone’s heart racing after taking an antibiotic they didn’t know could cause arrhythmias. Each case started with a decision that seemed fine at the time. But decisions in health need more than good intentions. They need clear facts, trusted sources, and systems that catch mistakes before they hurt you.
What follows is a collection of real, practical guides that expose these errors—and show you how to avoid them. You’ll find how to test a false allergy label, how to spot a fake pill, why your medication log might be useless, and how quality control failures happen behind the scenes. These aren’t theories. They’re lessons learned from patients, doctors, and manufacturers who’ve seen what happens when decisions go wrong. And more importantly, how to make them right.