Acute Hives: Causes, Triggers, and What to Do When They Strike
When your skin suddenly breaks out in raised, itchy red welts, you’re likely dealing with acute hives, a common skin reaction that appears suddenly and usually fades within days. Also known as urticaria, it’s not contagious, but it can feel terrifying—especially when it shows up out of nowhere after lunch, a walk outside, or a new pill. Unlike chronic hives that last weeks or months, acute hives last less than six weeks and often have a clear trigger you can track down.
Most cases of acute hives are tied to allergic reactions, the body’s overreaction to something harmless, like food, medicine, or insect bites. Common culprits include peanuts, shellfish, eggs, antibiotics like penicillin, and NSAIDs like ibuprofen. But not all hives are allergic. Viral infections—like the common cold or flu—can trigger them too. Even stress, heat, or tight clothing can set off a flare-up by causing histamine release, the chemical your immune system dumps into your skin to fight what it thinks is an invader. That release is what makes your skin swell and itch.
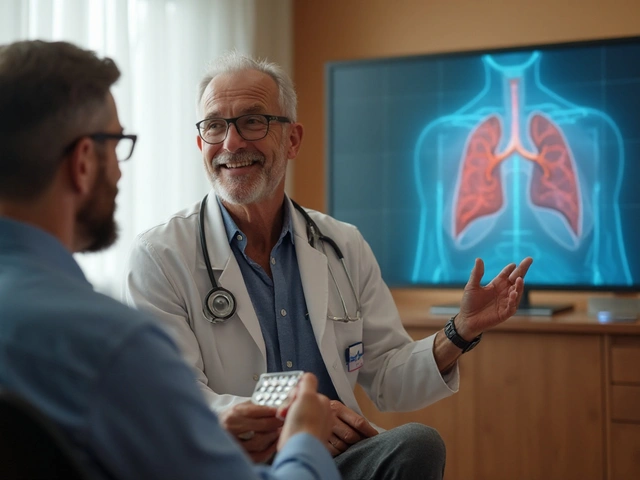
Here’s the good news: acute hives usually go away on their own. But that doesn’t mean you should ignore them. If you’re breaking out in hives after taking a new medication, stop it and call your doctor. If you feel swelling in your lips, tongue, or throat, or if you’re having trouble breathing, get emergency help—this could be anaphylaxis. For most cases, though, over-the-counter antihistamines like cetirizine or loratadine work fast. They block histamine before it causes more welts. Avoid scratching—it makes the itch worse and can lead to infection. Cool compresses and loose clothes help too.
What you won’t find in most guides is how often people misidentify the cause. You might blame your new detergent, but the real trigger could be the antibiotic you took three days ago. Or maybe it’s not an allergy at all—it’s a virus you didn’t even know you had. That’s why tracking your symptoms matters: what you ate, drank, touched, or took in the 24 hours before the hives showed up. Keep a simple log. It helps your doctor cut through the noise.
The posts below cover real cases and practical fixes. You’ll find how certain drugs like antihistamines can backfire if misused, why some people mistake hives for other rashes, and what to do when standard treatments don’t work. There’s also info on how to spot dangerous reactions that look like hives but aren’t—and how to avoid common mistakes that make things worse. No fluff. Just what works when your skin is on fire and you need answers fast.