Lopinavir/Ritonavir Drug Interaction Checker
Check Drug Interactions
Enter a drug name to see how it interacts with lopinavir/ritonavir and recommended adjustments.
Interaction Results
When doctors prescribe lopinavir/ritonavir for HIV, they’re not just giving two drugs-they’re setting off a chain reaction inside the body that affects nearly every other medication a patient might be taking. This isn’t just a minor side effect. It’s a powerful, unpredictable force that can turn a safe drug into a dangerous one-or make a life-saving treatment stop working altogether.
Why Ritonavir Is the Secret Weapon in Lopinavir Therapy
Lopinavir is an antiviral that fights HIV, but left on its own, it gets broken down too fast by the liver. Without help, you’d need to take it three times a day, and even then, levels in the blood might not be high enough to stop the virus. That’s where ritonavir comes in-not as a treatment for HIV, but as a chemical shield.
Ritonavir, given at just 100mg (one-quarter the dose used alone), blocks the enzyme CYP3A4. This enzyme is like a molecular shredder in the liver that breaks down hundreds of drugs, including lopinavir. When ritonavir shuts it down, lopinavir’s half-life jumps from under 7 hours to over 12. That means once-daily dosing becomes twice-daily, adherence improves, and viral suppression becomes more reliable.
This trick-called pharmacokinetic boosting-isn’t new. It was approved by the FDA in 2000 and became the backbone of HIV treatment for over a decade. But what made it revolutionary also made it risky: ritonavir doesn’t just block one enzyme. It messes with the whole system.
The Double-Edged Sword of Ritonavir’s Mechanism
Ritonavir doesn’t just inhibit CYP3A4-it destroys it. Unlike simple blockers that sit on the enzyme and wait, ritonavir gets metabolized into reactive pieces that latch onto CYP3A4 permanently. Think of it like pouring superglue into a machine. Once it’s glued, the enzyme can’t function anymore. This is called mechanism-based inactivation, and it’s why ritonavir is considered the strongest CYP3A4 inhibitor in clinical use.
But here’s the twist: ritonavir also turns on other enzymes. It induces CYP1A2, CYP2B6, CYP2C9, and CYP2C19. That means while it’s blocking some drugs, it’s speeding up the breakdown of others. This dual behavior creates a chaotic, unpredictable environment in the body.
Take warfarin, a blood thinner. Ritonavir induces CYP2C9, which breaks down warfarin faster. Patients on both drugs can suddenly find their INR levels dropping, putting them at risk for clots. Meanwhile, midazolam-a sedative used in surgery-is metabolized by CYP3A4. With ritonavir blocking that pathway, midazolam levels can spike by 500%. A normal dose becomes a near-overdose, leading to prolonged breathing problems.
This isn’t theoretical. In operating rooms across the world, anesthesiologists now routinely cut fentanyl and midazolam doses by 60-80% for patients on lopinavir/ritonavir. One wrong calculation, and a patient could stop breathing.
How Many Drugs Are Affected? The Numbers Don’t Lie
The Liverpool HIV Interactions Database, updated in July 2023, lists 1,247 potential drug interactions with lopinavir/ritonavir. That’s more than double the number for newer boosted regimens like darunavir/cobicistat.
Here’s what that means in practice:
- Tacrolimus (used after organ transplants): Levels increase 3-5 times. Without a 75% dose reduction, patients risk kidney failure.
- Rivaroxaban (a blood thinner): Contraindicated. The risk of internal bleeding is too high.
- Methadone: Ritonavir speeds up its breakdown. Doses often need to be increased by 20-33% to avoid withdrawal.
- Hormonal contraceptives: Effectiveness drops by over 50%. Backup contraception isn’t optional-it’s mandatory.
- Voriconazole (an antifungal): Levels become unpredictable. Sometimes too high (liver damage), sometimes too low (infection spreads). It’s contraindicated.
Even common OTC meds like St. John’s wort (used for mild depression) can crash lopinavir levels by 70%. That’s why every patient on this combo needs a full medication review before starting-and every new prescription after that must be checked again.

Why This Combo Is Still Used (Despite the Risks)
If it’s so dangerous, why is lopinavir/ritonavir still around?
Cost. In low- and middle-income countries, it costs $68 per person per year. Compare that to dolutegravir-based regimens, which run $287 annually. For programs like PEPFAR, which treats millions in sub-Saharan Africa, that difference is life or death.
It’s also reliable. In places without access to viral load testing, lopinavir/ritonavir has a long track record of keeping HIV suppressed-even when adherence isn’t perfect. And unlike some newer drugs, it doesn’t need refrigeration.
But even there, things are changing. UNAIDS predicts lopinavir/ritonavir’s global use will drop to 12% by 2027 as dolutegravir becomes more affordable. In the U.S., it’s used in less than 5% of new HIV cases. The CDC and DHHS guidelines now recommend integrase inhibitors as first-line for good reason: fewer interactions, fewer side effects, simpler management.
The Real-World Cost of Getting It Wrong
A 2022 meta-analysis found patients on lopinavir/ritonavir were 37% more likely to stop treatment because of side effects than those on newer drugs. That’s not just about nausea or diarrhea. It’s about liver damage, heart rhythm problems, and dangerous drug clashes.
One 2008 study showed that when patients on lopinavir/ritonavir also took rifampicin (for tuberculosis), their lopinavir levels dropped by 76%. Hepatotoxicity jumped from 11% to 33%. That’s not a coincidence-it’s a direct result of CYP3A4 induction overpowering ritonavir’s inhibition.
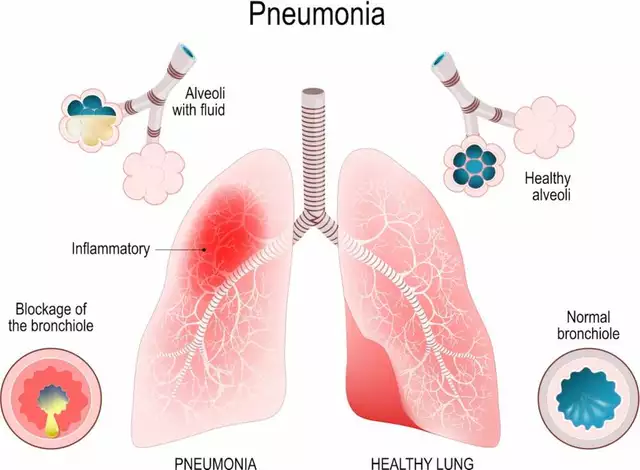
And it’s not just HIV patients. In the early days of the pandemic, lopinavir/ritonavir was tested for COVID-19. The RECOVERY trial in 2020 found zero benefit. Mortality was the same as standard care. But newer combinations like nirmatrelvir/ritonavir (Paxlovid) worked-because they used the same boosting principle on a different drug, with tighter control over dosing and timing.
Even Paxlovid isn’t perfect. The so-called “Paxlovid rebound”-where symptoms return after treatment-may be linked to ritonavir’s lingering effect on CYP3A4. Once ritonavir clears, the enzyme rebounds, and the antiviral gets broken down too fast. It’s a reminder: even when you know how the system works, it’s still hard to control.
What Clinicians Need to Do (And What They Often Skip)
There’s no magic bullet. The only way to avoid disaster is to treat every interaction like a live wire.
Every time a patient starts lopinavir/ritonavir, you need to:
- Get a complete list of all medications-prescription, OTC, supplements, herbal products.
- Check every single one against the Liverpool HIV Interactions Database (used over 2.8 million times a year).
- Look for both inhibition and induction risks. Don’t assume one effect dominates.
- Adjust doses proactively. Don’t wait for symptoms.
- Re-check every time a new drug is added-even an antibiotic or antacid.
Many providers skip step two. They assume “it’s just a booster,” or “it’s been used for years, it’s fine.” But the data doesn’t lie. Forty-eight percent of commonly prescribed drugs have a documented interaction. That’s nearly half of everything patients take.
And don’t forget liver function. Lopinavir/ritonavir carries a FDA black box warning for hepatotoxicity. Patients with pre-existing liver disease-especially hepatitis B or C-need lower doses or should avoid it entirely. Child-Pugh Class B patients get half the dose. Class C? Don’t use it.
The Future: Is There Still a Place for This Combo?
Lopinavir/ritonavir won’t disappear overnight. It’s too cheap, too stable, too proven in resource-limited settings. But its role is shrinking fast.
Research is now focused on how genetics play a role. Some people have a variant of CYP3A5 that breaks down lopinavir faster. Preliminary data shows these “expressers” have 28% lower drug levels. That means standard dosing might fail in a significant subset of patients.
Meanwhile, newer boosters like cobicistat are cleaner-they only block CYP3A4, with no induction effects. That’s why darunavir/cobicistat is now the gold standard in high-income countries. It’s not just safer. It’s simpler.
For now, lopinavir/ritonavir remains a tool-not a first choice. And like any powerful tool, it demands respect. Use it without understanding its interactions, and you’re not treating HIV. You’re gambling with lives.
Bottom Line: When in Doubt, Pause and Check
If you’re prescribing, dispensing, or taking lopinavir/ritonavir, remember this: ritonavir isn’t just a helper. It’s a gatekeeper that opens and closes doors in your body’s drug metabolism system. One wrong door, and something dangerous can slip through.
There’s no room for guesswork. Always check interactions. Always monitor. Always adjust. Because when CYP3A4 is involved, the smallest oversight can have the biggest consequences.





Post A Comment