Ocular Gonorrhea Symptom Checker
Check Your Symptoms
This tool compares your symptoms against the key indicators of ocular gonorrhea. Remember: this is not a diagnostic tool. If you have symptoms, see a healthcare provider immediately.
Symptoms to Watch For
Ocular gonorrhea symptoms typically appear within 24-48 hours and progress quickly. Check all symptoms you're experiencing.
Gonorrhea is a common sexually transmitted infection caused by the bacterium Neisseria gonorrhoeae. While most people think of genital symptoms, the bacteria can also invade the eye, leading to a condition known as ocular gonorrhea. This article breaks down who is at risk, what the eye looks like when it’s infected, how doctors confirm the diagnosis, and what you can do to get better fast.
What is ocular gonorrhea?
When Neisseria gonorrhoeae reaches the conjunctiva-the thin membrane covering the white of the eye and the inner eyelid-it triggers a rapid inflammatory response called gonococcal conjunctivitis. The infection can appear in newborns (often called ophthalmia neonatorum) or in adults who have transferred the bacteria from the genitals to the eye, usually via hands, towels, or sexual activity that involves contact with the eye.
How does the bacteria get to the eye?
- Direct contact: Touching the genitals and then the eye without washing hands.
- Sexual practices: Oralsex that includes contact with the eye or eyelids.
- Newborn exposure: During birth, a baby can be exposed if the mother’s birth canal is infected and prophylactic eye drops are missed.
- Contaminated objects: Sharing towels, makeup brushes, or contact lenses that have touched infected secretions.
Who is most at risk?
Anyone with an active gonorrhea infection can develop eye involvement, but certain groups face higher odds:
- Men who have sex with men (MSM): Higher rates of STI co‑infection increase the chance of ocular spread.
- Pregnant women: If untreated, they can pass the bacteria to the newborn.
- People with poor hand hygiene: Frequent touching of the eyes after genital contact.
- Contact lens wearers: Improper cleaning can create a moist environment for bacteria.
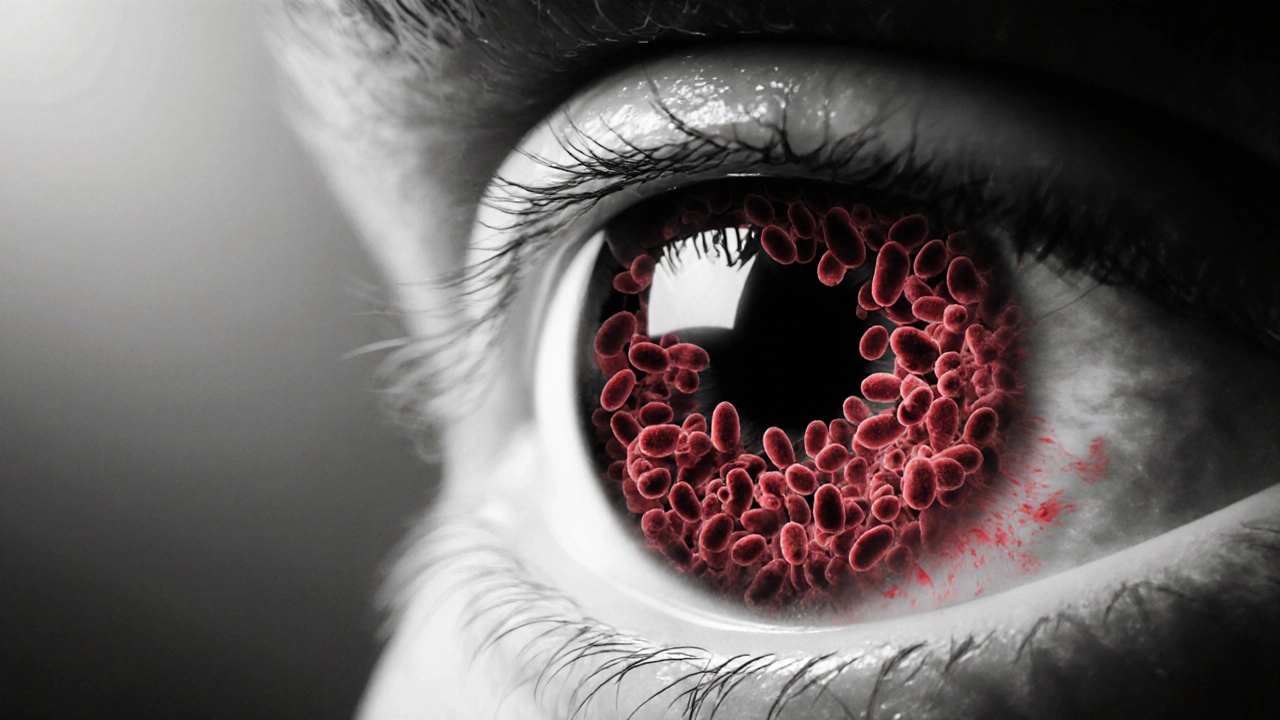
Symptoms to watch for
Gonococcal eye infection progresses quickly-often within 24‑48hours. Key signs include:
| Symptom | Description | Onset |
|---|---|---|
| Profuse purulent discharge | Thick, yellow‑green mucus that may crust eyelids | Hours |
| Redness (hyperemia) | Bright pink hue around the cornea and conjunctiva | Hours |
| Blepharospasm | Involuntary eyelid closing due to irritation | 1‑2days |
| Photophobia | Sensitivity to light, causing discomfort in bright rooms | 1‑2days |
| Corneal ulceration | Rare but serious; a sore spot on the cornea that can threaten vision | 2‑3days if untreated |

How doctors diagnose the infection
The diagnostic pathway is straightforward but must be done quickly:
- Clinical exam: An eye doctor (ophthalmologist or optometrist) looks for the classic thick discharge and conjunctival redness.
- Gram stain: A sample of the discharge is smeared on a slide; under a microscope, the characteristic kidney‑shaped diplococci of Neisseria gonorrhoeae appear.
- Culture or NAAT: The most reliable test uses a nucleic acid amplification test (NAAT) to detect bacterial DNA from the eye swab.
- Screening for other STIs: Because co‑infection with Chlamydia trachomatis is common, a concurrent urine or genital swab is often ordered.
Treatment protocols
Urgent antibiotic therapy is the standard of care. Current guidelines from the CDC and the WHO recommend a single intramuscular dose of ceftriaxone 500mg (1g for patients over 150kg) plus a single oral dose of azithromycin 1g to cover possible chlamydial co‑infection.
For the eye itself, doctors usually prescribe:
- Topical fluoroquinolone drops (e.g., ofloxacin) every hour for the first 24hours, then tapering over 5‑7days.
- Warm compresses to help clear crusted discharge.
Follow‑up is essential. If symptoms persist after 48hours, a repeat culture should be performed to rule out antibiotic‑resistant strains.
Preventing ocular spread
Prevention boils down to two pillars: controlling the primary infection and practicing good eye hygiene.
- Get tested regularly: Annual STI screening for sexually active adults, and immediate testing after any unprotected encounter.
- Treat partners: Simultaneous therapy for all sexual partners reduces reinfection risk.
- Hand washing: Wash hands with soap for at least 20seconds before touching your face or eyes.
- Avoid sharing personal items: Towels, pillowcases, makeup, and contact lens cases should be personal.
- Newborn prophylaxis: In many countries, a single dose of erythromycin eye ointment is applied within one hour after birth; ensure this step isn’t missed.

When to seek immediate medical help
If you notice any of the following, head to an urgent‑care clinic or emergency department:
- Rapidly increasing discharge that makes it hard to keep the eye open.
- Severe pain, vision blurry, or a feeling of a foreign body.
- Signs of corneal ulcer (white spot on the clear part of the eye).
Delayed treatment can lead to permanent scarring, reduced vision, or even blindness.
Key takeaways
- Ocular gonorrhea is a fast‑acting eye infection that stems from the same bacteria that cause genital gonorrhea.
- Symptoms appear quickly and include thick yellow‑green discharge, redness, and possible corneal damage.
- Diagnosis relies on a clinical exam plus Gram stain or NAAT of eye secretions.
- Single‑dose ceftriaxone plus azithromycin, plus topical antibiotics, clears the infection in most cases.
- Good hand hygiene, regular STI testing, and prompt treatment of partners are the best defenses.
Frequently Asked Questions
Can gonorrhea affect only one eye?
Yes. It often starts in one eye, especially if the infection was transferred by touching a single eye. However, without treatment it can quickly spread to the other eye.
Is ocular gonorrhea contagious to others?
The eye discharge contains live bacteria, so direct contact with the secretions can transmit the infection. Practicing hand washing and not sharing towels eliminates the risk.
How long does treatment take to work?
Systemic antibiotics start killing the bacteria within hours. Most patients notice reduced discharge and redness within 24‑48hours, but the full course of eye drops should be completed to prevent recurrence.
Can I use over‑the‑counter eye drops for relief?
Artificial tears can soothe irritation, but they won’t treat the bacterial cause. Using them without antibiotics may delay proper treatment and increase the risk of complications.
What if I’m allergic to ceftriaxone?
Allergy to cephalosporins is rare but documented. Alternatives include a single dose of spectinomycin (if available) or a higher‑dose fluoroquinolone regimen, but these should be chosen by a specialist.





Post A Comment