When you hear the word generic, you probably think of cheap pills you pick up at the pharmacy for $4. But when it comes to biologic drugs, the story changes. There’s no such thing as a true generic version of a biologic. Instead, there are biosimilars - highly similar, but not identical, copies. And the cost difference between these biosimilars and the original brand-name biologics is one of the biggest financial shifts in modern medicine.
What Exactly Is a Biologic?
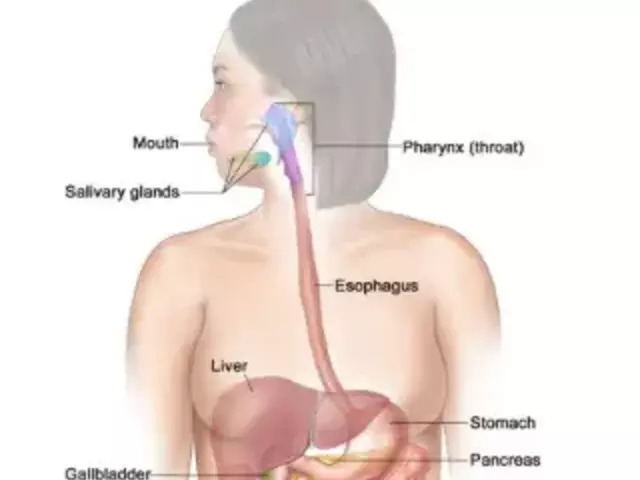
Biologics aren’t made in a lab like regular pills. They’re produced using living cells - bacteria, yeast, or animal cells - to create complex proteins that treat conditions like rheumatoid arthritis, Crohn’s disease, cancer, and diabetes. Because they’re made from living systems, no two batches are exactly the same. That’s why you can’t just copy them like you would aspirin or metformin. These drugs are powerful. They’re also expensive. In 2024, biologics made up only 5% of all prescriptions in the U.S., but they accounted for 51% of total drug spending. That’s $1 out of every $2 spent on medicine going to just one-fifth of the prescriptions.Why Biosimilars Are Different from Regular Generics
Regular generics are exact chemical copies of brand-name drugs. If your doctor prescribes Lipitor, the generic atorvastatin has the same active ingredient, same dose, same shape, same everything. It’s a direct replacement. Biosimilars? Not the same. They’re designed to be highly similar to the original biologic, with no clinically meaningful differences in safety or effectiveness. But because they’re made from living organisms, tiny variations in manufacturing can lead to minor structural differences. That’s why they can’t be called “generics.” They’re biosimilars - a new category. The FDA approved the first biosimilar, Zarxio (a copy of filgrastim), in 2015. Since then, 76 biosimilars have been approved as of October 2025. That sounds like a lot - until you realize there are about 600 biologics on the market. Only a small fraction have biosimilar alternatives.The Real Cost Difference: Numbers That Matter
Let’s cut through the noise. Here’s what the data shows in 2025:- Brand biologic average 30-day cost: $2,104
- Biosimilar average 30-day cost: $919
How Much Have Biosimilars Saved So Far?
Since 2015, biosimilars have saved the U.S. healthcare system between $36 billion and $56 billion, depending on who’s counting. The Association for Accessible Medicines (AAM) says total savings from all generics and biosimilars hit $445 billion in 2023 alone. That’s not a typo. $445 billion in one year. In 2024, biosimilars saved $20 billion. That’s enough to cover the annual cost of care for tens of thousands of patients who couldn’t afford their meds before. But here’s the problem: despite these savings, biosimilars still make up less than 20% of the biologic market. Compare that to traditional generics, which account for 90% of prescriptions but only 13% of spending. Why the gap?Why Aren’t More People Using Biosimilars?
It’s not because they’re unsafe. The FDA says approved biosimilars are as safe and effective as the originals. Doctors and patients just don’t use them as much - and here’s why:- Patent thickets: Brand companies file dozens of patents on small changes to the drug or its delivery system. These aren’t real innovations - they’re legal roadblocks. One biologic can have over 100 patents, making it nearly impossible for biosimilar makers to enter without getting sued.
- Rebate walls: Pharmacy Benefit Managers (PBMs) get huge rebates from brand-name drugmakers to keep their products on the preferred list. Those rebates often go to the PBM, not the patient or insurer. So even if a biosimilar is cheaper, the system still pushes the more expensive option.
- Slow adoption by insurers: Many health plans still require patients to try the brand drug first - even if it’s twice as expensive - before approving the biosimilar.
- Cost of development: Creating a biosimilar costs $100-250 million. That’s a huge barrier for smaller companies. Big pharma has the resources to fight patents and lawsuits. Smaller players don’t.
What’s Changing? The Future of Biosimilars
The FDA is finally pushing to make biosimilar development faster and cheaper. In September 2025, they released new draft guidance to reduce unnecessary clinical trials. That could cut development time by years and lower costs. The Biden administration’s Biosimilars Action Plan aims to remove barriers to access, including fixing rebate structures and encouraging insurers to prioritize biosimilars. Industry analysts predict biosimilar market share will jump from 15-20% today to 35-40% by 2030. That could mean $125 billion in annual savings - enough to cover the cost of insulin for every diabetic in the U.S. for years.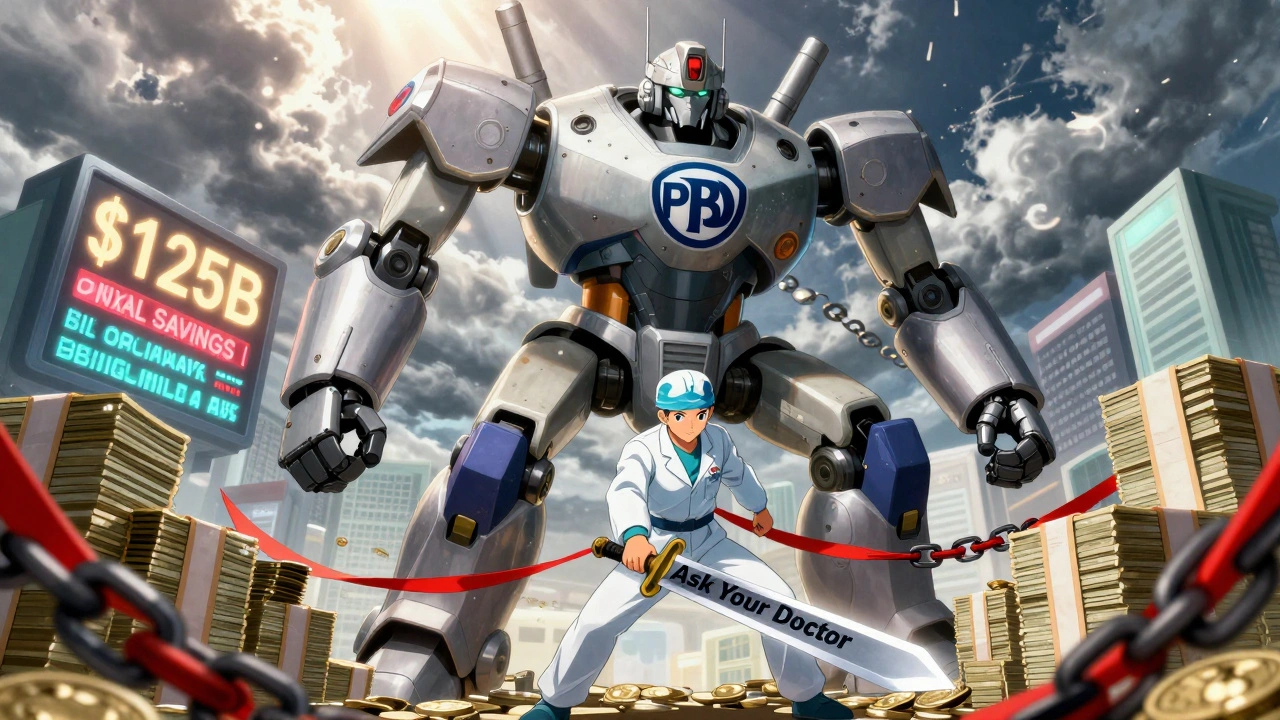
What This Means for You
If you’re taking a biologic right now - whether it’s for arthritis, psoriasis, or cancer - ask your doctor or pharmacist: “Is there a biosimilar available?” You might be paying three times more than you need to. Switching isn’t always automatic. Sometimes you need to ask. Sometimes you need to fight. But the savings are real. And the science is solid. Don’t assume your insurance will switch you automatically. Don’t assume your doctor knows all the options. Take control. Ask. Check. Compare. The system is rigged to keep prices high. But you don’t have to be part of that equation.Is a Biosimilar Right for Everyone?
Most patients can safely switch. Clinical trials show no difference in outcomes. But if you’ve been stable on a brand biologic for years, and your doctor says there’s no reason to change, that’s fine. The goal isn’t to switch for the sake of switching. It’s to avoid paying more than you have to. If you’re on Medicare Part D, the Inflation Reduction Act caps insulin at $35 per month - but that cap doesn’t apply to most other biologics. Biosimilars are your best shot at lowering costs for those drugs.Bottom Line
Brand biologics aren’t expensive because they’re better. They’re expensive because they can be. Biosimilars prove that you don’t need to pay $80,000 a year for a drug that works just as well at $16,000. The savings are massive. The science is clear. The barriers are political and financial - not medical. You have the power to ask for a cheaper, equally effective option. Use it.Are biosimilars as safe as brand biologics?
Yes. The FDA requires biosimilars to show no clinically meaningful differences in safety, purity, or potency compared to the original biologic. Thousands of patients have used biosimilars since 2015, and post-market monitoring shows no increase in adverse events. In fact, the FDA states that approved biosimilars are as safe and effective as their brand-name counterparts.
Why are biosimilars cheaper if they’re so complex to make?
Biosimilars don’t need to repeat all the expensive clinical trials the original brand did. They rely on the brand’s existing safety and efficacy data, which cuts development time and cost. While developing a biosimilar still costs $100-250 million, that’s far less than the $1-2 billion it takes to bring a new biologic to market. Plus, competition drives prices down further.
Can I switch from a brand biologic to a biosimilar on my own?
No. You should never switch without consulting your doctor. Even though biosimilars are safe and effective, your doctor needs to approve the change, update your prescription, and monitor your response. Some insurers require prior authorization. Your pharmacy can help you navigate the process, but don’t switch without medical oversight.
Do biosimilars work as well for cancer treatment?
Yes. Several biosimilars are approved for cancer treatments, including drugs like bevacizumab (Avastin biosimilars) and trastuzumab (Herceptin biosimilars). Studies show they have the same response rates, survival outcomes, and side effect profiles as the original drugs. Many cancer centers now use biosimilars as standard of care because they offer the same results at lower cost.
Why isn’t my insurance covering the biosimilar?
Many insurers still favor brand biologics because of rebate deals with drugmakers. PBMs get paid more to keep expensive drugs on formularies, even if cheaper alternatives exist. Ask your pharmacy to submit a prior authorization for the biosimilar. If denied, appeal. You can also ask your doctor to write a letter of medical necessity. Many appeals are successful when backed by clinical evidence.
Will biosimilars eventually replace brand biologics entirely?
Not entirely - but they will dominate the market. By 2030, analysts predict biosimilars will make up 35-40% of the biologic market. That’s still not 100%, but it’s enough to drive prices down permanently. The original brands will likely remain for patients who don’t respond to biosimilars or have rare conditions. But for most people, biosimilars will become the default choice.




Post A Comment