Emphysema Oxygen Therapy Calculator
Oxygen Therapy Assessment
Estimate your oxygen therapy needs based on activity level and current usage. This tool provides general guidance only - always consult your doctor for personalized recommendations.
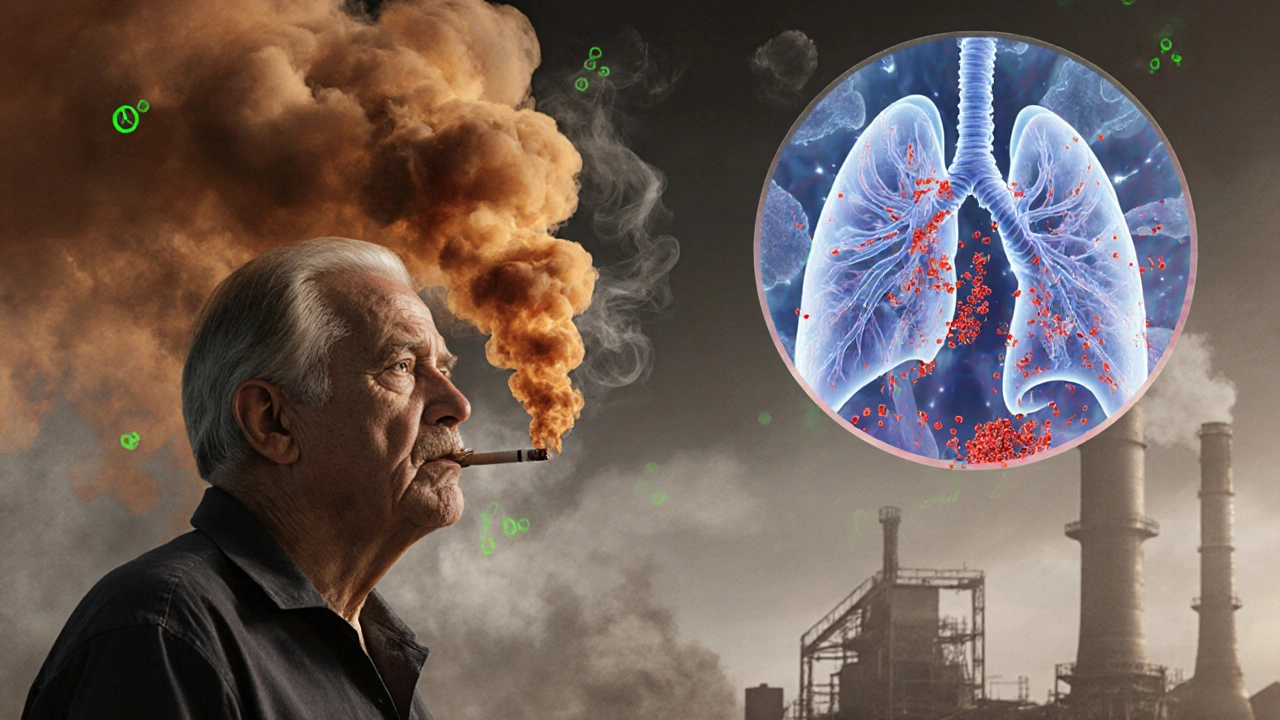
When doctors talk about chronic lung disease, Emphysema is a condition that destroys the air‑sac walls (alveoli) in the lungs, making it hard to move oxygen into the bloodstream. It’s the “air‑sac‑damage” half of chronic obstructive pulmonary disease (COPD) and affects millions worldwide. This guide breaks down what causes it, how you’ll know you have it, and which treatments actually help you breathe easier.
What Is Emphysema?
COPD is a group of progressive lung diseases that block airflow and make breathing difficult, and emphysema is the component that destroys the tiny air sacs. When the sacs burst, the lungs lose elasticity, air gets trapped, and the chest takes on a “barrel” shape. The damage is permanent, but early detection and proper care can slow the decline.
Primary Causes
- Smoking is the leading cause of emphysema, responsible for roughly 85% of cases worldwide. The smoke’s chemicals irritate and inflame the airway walls, accelerating alveolar destruction.
- Environmental pollutants such as ozone, sulfur dioxide, and fine particulate matter can worsen lung inflammation, especially in urban areas.
- Alpha‑1 antitrypsin deficiency is a rare genetic disorder that reduces a protein protecting the lungs from enzyme damage. Even non‑smokers with this condition can develop emphysema early.
- Occupational exposure to dust, silica, or chemicals (e.g., coal mining, construction) adds a cumulative risk.
Most people who develop emphysema have more than one risk factor - a smoker who works in a dusty environment is especially vulnerable.
How the Damage Happens
In healthy lungs, elastic fibers keep alveoli springy. Harmful particles trigger an immune response that releases enzymes called elastases. Over time, these enzymes break down the elastic tissue. Without elasticity, alveoli can’t recoil, air remains trapped, and the lungs over‑inflate.
Spotting the Symptoms
- Shortness of breath, especially during physical activity, is often the first sign.
- A chronic, dry cough that may produce little or no mucus.
- Wheezing or a whistling sound when breathing out.
- Frequent respiratory infections - the damaged lungs struggle to clear germs.
- Barrel‑shaped chest: the ribs become more horizontal as the lungs expand.
- Unintentional weight loss, known as “pink‑puffer” syndrome, where patients appear thin despite eating normally.
Symptoms often develop slowly, which is why many people don’t realize they have emphysema until a routine check‑up reveals abnormal lung function.
How Doctors Diagnose It
The gold‑standard test is spirometry which measures how much air you can force out of your lungs and how fast you can do it. A reduced FEV1/FVC ratio (less than 0.7) points to COPD. Doctors may also order a chest X‑ray or CT scan to visualize lung tissue and rule out other issues. Blood tests can check for alpha‑1 antitrypsin levels when a genetic cause is suspected.
Treatment Options
While no cure exists, several therapies improve quality of life, reduce flare‑ups, and extend survival.
| Treatment | How It Works | Typical Use | Key Benefits | Potential Side Effects |
|---|---|---|---|---|
| Bronchodilators | Relax airway muscles | Every day, as inhaler | Quick relief of breathlessness | Tachycardia, hand tremor |
| Inhaled corticosteroids | Reduce airway inflammation | Often combined with bronchodilators | Fewer exacerbations | Oral thrush, hoarse voice |
| Oxygen therapy | Supplies extra oxygen to blood | Continuous or nocturnal | Improves stamina, lowers heart strain | Dry nasal passages, fire risk |
| Pulmonary rehabilitation | Exercise, education, breathing techniques | Program lasting 6‑12 weeks | Better exercise tolerance, mood boost | Fatigue during early sessions |
| Lung‑volume‑reduction surgery | Removes damaged lung tissue | Selected severe cases | Significant airflow improvement | Infection, air leak, surgery risk |
| Lung transplant | Replaces both lungs with donor organs | End‑stage disease | Potential for normal life expectancy | Immune rejection, lifelong meds |
Choosing the right mix depends on disease severity, lifestyle, and other health issues. Your pulmonologist will tailor a plan that balances relief with side‑effect risk.

Living Strategies & Prevention
- Quit smoking: The single most effective step. Resources include nicotine patches, prescription meds, and counseling. A typical quit plan:
- Set a quit date within the next two weeks.
- Identify triggers (coffee, stress) and replace them with healthier habits.
- Use a nicotine replacement product for 8‑12 weeks.
- Seek support from a quit‑line or local group.
- Get vaccinated yearly against influenza and once against pneumonia - infections can cause dangerous flare‑ups.
- Practice breathing exercises such as pursed‑lip breathing to slow exhalation and keep airways open.
- Stay active: moderate walking or cycling improves lung capacity and heart health.
- Maintain a healthy weight. Rapid weight loss can worsen breathlessness, while obesity adds extra strain.
Even after diagnosis, these habits can slow the disease and improve daily comfort.
Managing Daily Life
Emphysema can be unsettling, but a few practical steps make a big difference.
- Carry a rescue inhaler and know when to use it (sudden breathlessness).
- Monitor oxygen levels with a pulse oximeter; aim for 90%‑95% at rest.
- Plan activities around energy levels - schedule demanding tasks for times when you feel strongest.
- Keep a symptom diary: note breathlessness, cough, or medication changes. This data helps doctors adjust treatment.
- Consider mental‑health support. Dealing with a chronic illness can trigger anxiety or depression; counseling or support groups are valuable.
Frequently Asked Questions
Can emphysema be reversed?
No. The damage to alveoli is permanent. However, quitting smoking, using medication, and staying active can halt further loss and improve symptoms.
Is shortness of breath always a sign of emphysema?
Shortness of breath can stem from many conditions, such as asthma, heart failure, or anemia. A spirometry test is needed to confirm emphysema.
How often should I see my doctor?
At least once a year for routine monitoring. If you notice a sudden increase in symptoms or need new medication, schedule an appointment promptly.
Are there any new treatments on the horizon?
Researchers are testing stem‑cell therapy and novel anti‑elastase drugs. While promising, these are still in clinical trials and not yet widely available.
Can exercise make emphysema worse?
When done correctly, exercise strengthens respiratory muscles and improves endurance. Over‑exertion without proper pacing can cause fatigue, so start slow and follow a pulmonary rehab program.




Post A Comment