Proctitis and Food Allergies: How They’re Linked
Explore how food allergies can trigger proctitis, learn to spot common allergens, get diagnostic tips, and discover diet and treatment strategies.
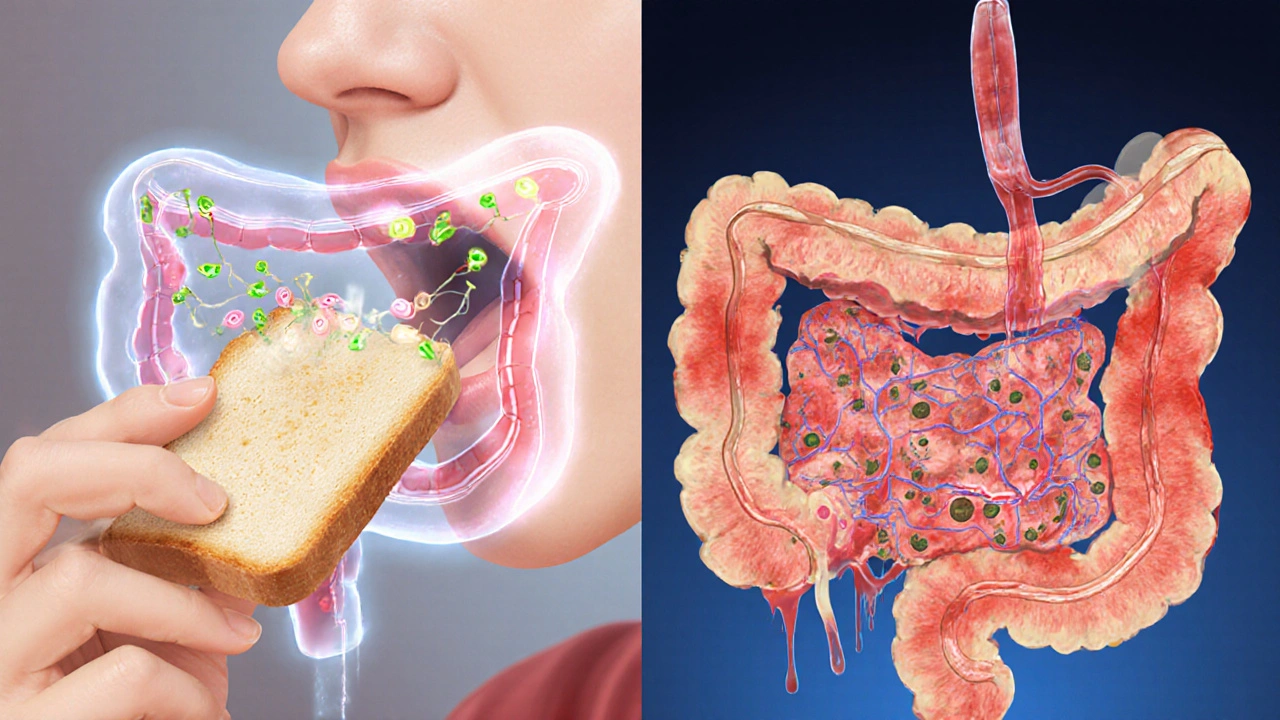
When working with Inflammatory Bowel Disease, a chronic condition that triggers inflammation in the intestines, often causing pain, diarrhea, and fatigue. Also known as IBD, it Inflammatory bowel disease covers several disorders, the most common being Crohn's disease, an IBD type that can affect any part of the gastrointestinal tract from mouth to anus and Ulcerative colitis, a form that limits inflammation to the colon and rectum. Both share symptoms like abdominal cramping and weight loss, yet they differ in location and severity. Understanding these nuances helps you pick the right treatment plan.
Managing IBD often means combining medication, lifestyle tweaks, and nutrition strategies. A key drug for mild‑to‑moderate cases is Budesonide, marketed as Entocort, which works locally in the gut to reduce inflammation with fewer systemic side effects than traditional steroids. Patients typically use budesonide during flare‑ups, then taper off as symptoms improve. The drug’s targeted action exemplifies how modern therapy aims to balance efficacy and safety, a major goal for anyone dealing with chronic gut issues.
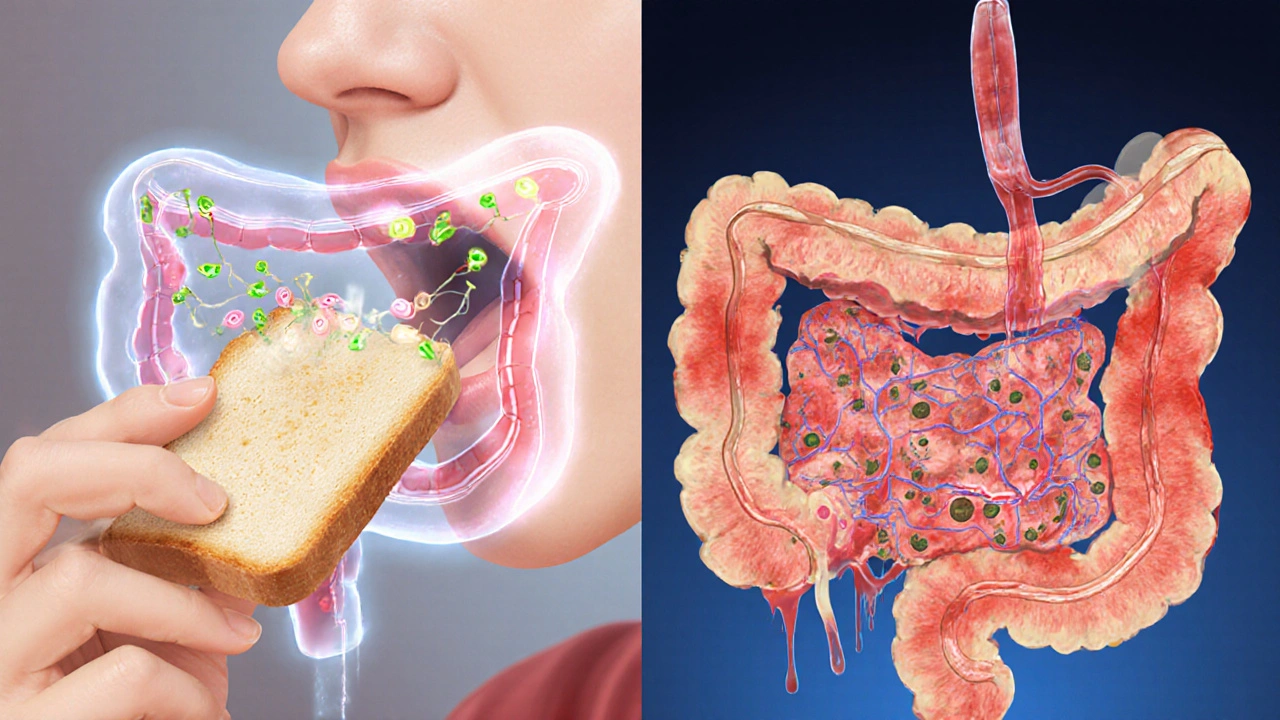
Food isn’t just fuel; it can trigger or soothe IBD flare‑ups. A high‑fiber, low‑irritant diet supports gut lining, promotes regular bowel movements, and may lower the risk of complications like hemorrhoids, which some IBD sufferers experience due to chronic diarrhea. Incorporating soluble fiber from oats, bananas, and peeled apples can be gentler than insoluble sources like raw broccoli. Staying hydrated and limiting caffeine, alcohol, and spicy foods also reduces irritation. These practical steps are backed by nutritionists who see fewer emergency visits when patients stick to a balanced, gut‑friendly menu.
Beyond fiber, anti‑inflammatory foods such as omega‑3‑rich fish, turmeric, and leafy greens can complement medication. While no single diet cures IBD, a consistent eating plan makes it easier to track triggers. Many patients keep a food diary, noting what they ate and how they felt later. Over time this data uncovers patterns—like a specific spice causing pain—allowing personalized adjustments without trial‑and‑error chaos.
Exercise also plays a subtle role. Moderate activities like walking or yoga improve circulation, reduce stress, and may lower inflammation markers. Stress alone can worsen IBD symptoms, so combining movement with relaxation techniques creates a holistic approach that many clinicians recommend alongside budesonide or other prescriptions.
When flare‑ups happen, short‑term strategies become crucial. Over‑the‑counter options like antidiarrheal agents can provide temporary relief, but they shouldn’t replace prescribed meds. Instead, they buy you time while adjusting your budesonide dose or contacting your doctor. Knowing when to step up treatment versus when to manage symptoms at home is a skill that comes with experience and good medical guidance.
For those newly diagnosed, the learning curve can feel steep. Understanding that IBD is a lifelong condition, not a one‑time illness, helps set realistic expectations. Regular check‑ups, blood work, and colonoscopies track disease activity and guide adjustments to medication or diet. Early detection of complications—like strictures or fistulas—means faster intervention and better outcomes.
In short, mastering Inflammatory Bowel Disease involves three pillars: effective medication such as budesonide, a gut‑friendly diet rich in soluble fiber and anti‑inflammatory foods, and lifestyle habits that keep stress low and activity steady. Below you’ll find a curated list of articles that dive deeper into each pillar—comparisons of IBD drugs, recipe ideas for a calmer gut, and practical buying guides for the meds you may need. Browse through to find the exact tip or insight you’re looking for, and feel empowered to take charge of your health.
Explore how food allergies can trigger proctitis, learn to spot common allergens, get diagnostic tips, and discover diet and treatment strategies.