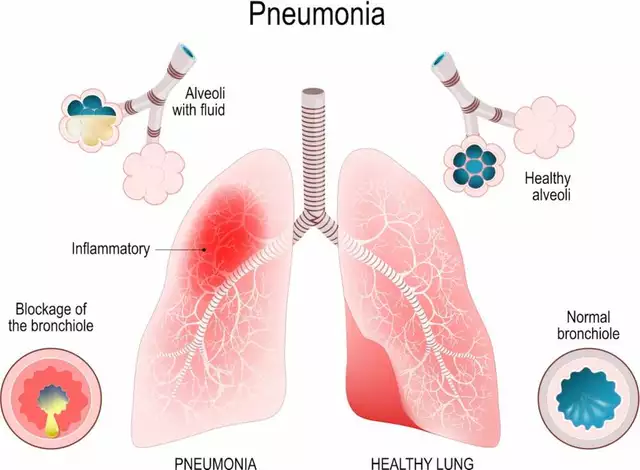
When a batch of medicine is released to patients, no one should be asking, "Who really said it was safe?" That’s the core question behind quality assurance units - and why their independence isn’t just a best practice, it’s a legal requirement in regulated industries like pharmaceuticals and nuclear energy.
What Exactly Is a Quality Assurance Unit?
A quality assurance unit (QU) is a formally recognized team with the legal authority to approve or reject every step of a production process. It doesn’t make the product. It doesn’t run the machines. It doesn’t meet production targets. Its only job is to make sure everything done to make the product meets strict quality standards - and to say "no" when it doesn’t. This isn’t a suggestion. Under FDA regulations (21 CFR 211.22), the quality control unit must have "the responsibility and authority to approve or reject all components, drug product containers, closures, in-process materials, packaging material, labeling, and drug products." In plain terms: if the QU says a batch is unsafe, it doesn’t get shipped. Period. The difference between quality assurance (QA) and quality control (QC) matters here. QA looks at the system - the procedures, the training, the documentation. QC looks at the product - testing samples, checking labels, verifying measurements. But both must be independent of production to work.Why Independence Isn’t Optional
Imagine a factory manager under pressure to hit monthly targets. The production line is running slow. A sensor flags a minor deviation in temperature during mixing. The operator says it’s "within tolerance." The production team wants to push through. But the quality team knows the deviation could affect potency. If the quality team reports to that same manager - who’s being judged on output - what happens? The pressure to say "yes" grows. The batch gets released. A patient gets sick. The company gets a warning letter. And the regulator finds out the QU had no real power to stop it. That’s not hypothetical. In 2024, 68% of FDA warning letters issued to pharmaceutical manufacturers cited failures in quality unit independence. Many involved situations where the QU was buried under production leadership - reporting to a plant manager, not the CEO. That’s a conflict of interest waiting to happen. The FDA is clear: "Quality decisions must remain objective and focused on product quality rather than production metrics or efficiency considerations." Independent oversight means the QU answers to someone who cares more about safety than speed.How Independence Works in Practice
A compliant QU doesn’t just sit in an office. It has real power:- It can halt production on the spot if a critical deviation occurs.
- It must review and approve every batch record before release.
- It audits production processes regularly - not just when something goes wrong.
- It has direct access to the CEO or Board of Directors without going through production managers.
What Happens When Independence Fails
Small companies are especially vulnerable. FDA data shows 42% of warning letters to facilities with fewer than 50 employees involve QU independence issues. Why? Budgets are tight. One person wears too many hats. The production manager also serves as QA manager. It’s efficient - until it’s not. Reddit user "QualityAssurancePro" described exactly this in 2024: "My company tried to have the production manager also serve as QA manager during restructuring. Within 3 months, we had two critical deviations that weren’t properly investigated before batch release." That’s not a mistake. That’s systemic failure. Another red flag: QU-to-production staff ratios below 1:15. When one quality person is responsible for checking 15 production staff, they’re overwhelmed. They start rubber-stamping documents just to keep up. FDA data shows these facilities have 3.2 times more repeat deviations. The cost? Not just fines. Lost trust. Patient harm. Brand damage. And in pharmaceuticals, that’s not abstract - it’s life or death.How Large Companies Get It Right
Big players like Merck and Eli Lilly don’t cut corners. Merck spent nine months restructuring its QU reporting lines in 2023. Production leaders resisted. There were meetings. Tensions. But they stuck to the rule: no production manager can approve a quality decision. Eli Lilly introduced "quality ambassadors" - production staff trained in quality principles, but still separate from the QU. The result? A 40% improvement in quality culture. People started speaking up. Problems got flagged earlier. These companies also have clear "quality hold" procedures. If a batch is flagged, the QU can freeze it without asking permission. The system is designed to bypass production management entirely. Ninety-two percent of organizations with zero FDA 483 observations have this in place.The Numbers Don’t Lie
Here’s what real-world data shows:- Organizations with independent QUs have 28% faster resolution of critical quality deviations.
- First-time inspection success rates are 31% higher when QU independence is enforced.
- 63% of warning letters for data integrity violations come from companies with integrated quality-production teams.
- QU staff average 8.2 years of industry experience and must be trained in GMP, statistical process control, and conflict resolution.

What’s Changing Now?
Digital manufacturing is shaking things up. AI systems now make real-time quality decisions - adjusting temperature, flow rates, mixing times on the fly. But who’s watching the AI? If the same team that runs production also programs the AI, the independence is gone. In January 2025, the FDA released draft guidance on "Quality Unit Independence in Digital Manufacturing Environments." The message: even if decisions are automated, the oversight must still be separate. Algorithms can’t replace human judgment - especially when safety is on the line. The European Commission’s 2024 update to EudraLex made it even clearer: "Quality units shall not be organizationally subordinate to production departments under any circumstances." No exceptions. No loopholes.What You Can Do
If you work in manufacturing - especially pharma, medical devices, or nuclear - here’s what you need to check:- Where does your QU report? If it’s under production, it’s not independent.
- Can your QU halt production without approval from a production manager?
- Is there a documented "quality hold" procedure that bypasses production leadership?
- Do QU staff have direct access to the CEO or Board?
- Is the QU staffed enough? Are they overwhelmed?
- Are they trained in conflict resolution? They’ll need it.
Bottom Line
Quality assurance units aren’t a cost center. They’re a safety net. They’re the last check before something reaches a patient, a soldier, or a nuclear reactor. When independence is compromised, the risk isn’t just regulatory. It’s human. The data doesn’t lie. Independent oversight reduces failures. Speeds up fixes. Builds trust. And in regulated industries, that’s not optional - it’s the law.Can a production manager also be the quality assurance manager?
No. Regulatory agencies like the FDA and EMA explicitly prohibit this. When one person controls both production targets and quality decisions, conflicts of interest are inevitable. The QU must be organizationally separate. Even if one person holds both titles, another qualified individual not involved in production must periodically review their quality decisions to maintain independence.
What happens if the quality unit approves a bad batch?
If a batch is released and later found to be unsafe, the entire quality unit is subject to regulatory scrutiny. Investigators will look at whether the QU had the authority to stop it, whether they were pressured, and whether their procedures were followed. In many cases, the entire leadership team - including the CEO - can be held accountable. The FDA has issued warning letters and even injunctions against companies where quality units failed to act.
How small can a company be and still have a compliant quality unit?
There’s no minimum size, but small companies face higher risks. Even a team of two can be compliant if one person is fully dedicated to quality and reports directly to the owner or board. However, FDA data shows 42% of independence violations occur in facilities under 50 employees. Many small firms use third-party quality oversight services to meet requirements without hiring full-time staff.
Do quality assurance units have the power to fire people?
No, the QU does not have hiring or firing authority. But they can recommend disciplinary action if someone repeatedly ignores quality procedures or falsifies records. In serious cases, they can escalate to senior leadership or the board - who do have the power to terminate. Their real power lies in refusing to release product, shutting down lines, or triggering regulatory investigations.
Is quality assurance the same as quality control?
No. Quality assurance (QA) focuses on the system - the processes, training, documentation, and audits. Quality control (QC) focuses on the product - testing samples, checking measurements, verifying labels. Both are part of the quality unit, but QA ensures the system works, while QC checks the output. Both must be independent to be effective.


Post A Comment