SGLT2 Infection Risk Calculator
This calculator estimates your risk of genital infection based on your SGLT2 inhibitor medication, dose, and gender using clinical trial data from the article.
Enter your medication details and click "Calculate Your Risk" to see your estimated infection risk.
Important Note: Following proper hygiene practices (rinsing after voiding and before bed) can reduce infection risk by about 40% as shown in the article.
When taking SGLT2 inhibitors are oral diabetes medicines that block the sodium‑glucose cotransporter‑2 in the kidneys, causing excess glucose to be expelled in the urine, many patients notice a sweet side effect: more sugar in the pee. That extra sugar fuels genital mycotic infections, especially in people with type 2 diabetes mellitus. Below is a step‑by‑step guide to keep those infections at bay without giving up the cardiovascular and renal benefits of the drugs.
Quick Takeaways
- Rinse the genital area with water after every void and before bed - it cuts infection rates by about 40%.
- Drink 2-3 L of fluid daily to dilute urine glucose.
- Choose cotton underwear and avoid tight clothing for better ventilation.
- Know the drug‑specific risk: canagliflozin has the highest infection rate, followed by dapagliflozin and empagliflozin.
- Seek medical help if redness spreads, pain worsens, or you notice foul odor - it could be Fournier's gangrene.
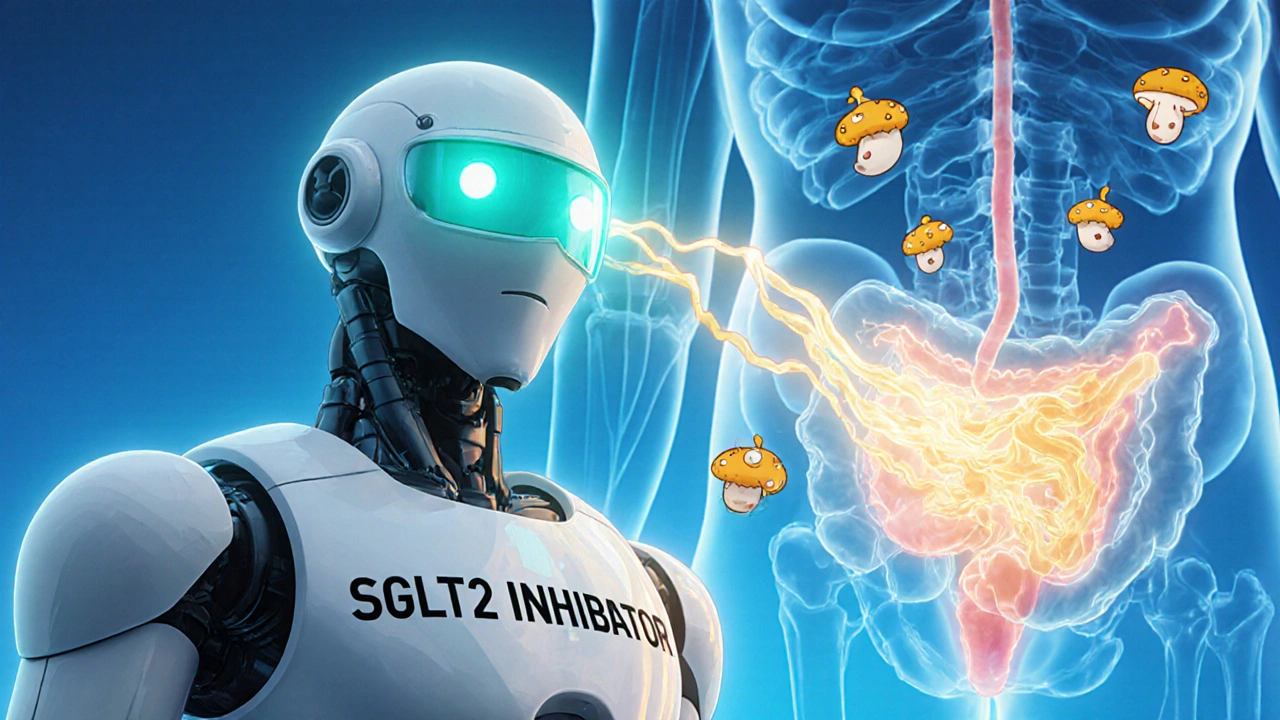
Why SGLT2 Inhibitors Increase Infection Risk
The core reason is glucosuria. By preventing glucose reabsorption, these drugs push 30-80 g of sugar into each urine stream. Sugar is a perfect food for Candida species, the fungus behind most genital mycotic infections. Warm, moist skin around the genitals becomes a breeding ground, especially when hygiene lapses occur.
Studies show a three‑fold rise in infection rates versus other diabetes meds. Women on SGLT2 inhibitors experience infections in 4-12 % of cases, men in 2-5 % (Engelhardt et al., 2020). The risk rises with higher doses - canagliflozin 300 mg produced a 12.3 % infection rate in women versus 8.7 % at 100 mg.
Drug‑Specific Infection Profiles
| Drug | Female infection rate | Male infection rate | Notes |
|---|---|---|---|
| Canagliflozin | 10-12 % | 4-6 % | Highest risk, dose‑dependent |
| Dapagliflozin | 8-10 % | 2-4 % | Lower than canagliflozin |
| Empagliflozin | 8-9 % | 2-3 % | Similar to dapagliflozin |
Even though the numbers differ, the principle stays the same: more sugar in the urine, higher infection chance.
Hygiene: The First Line of Defense
Cleaning the genital area with water after every void is the simplest, most effective habit. The American Diabetes Association (ADA) rates this recommendation as a grade B intervention.
- Finish urinating.
- Use a gentle stream of lukewarm water to rinse the front‑to‑back (for women) or retract the foreskin and rinse (for uncircumcised men).
- Pat dry with a clean, soft towel - avoid rubbing.
- Put on fresh cotton underwear before leaving the bathroom.
Doing the same routine before bedtime adds a second protective window, because the night’s long sleep period otherwise lets glucose sit on the skin.
Hydration: Diluting the Sugar
Drinking enough fluid reduces the concentration of glucose in each bladder fill. A practical target is 2-3 L (about 8-12 cups) of water daily, split across meals and between‑meal snacks. For people on diuretics or with heart failure, adjust the fluid goal with your clinician.
Research hasn’t measured exact concentration thresholds, but real‑world observations link higher fluid intake with a 15 % drop in infection recurrence.
Timing Matters: When to Clean and When to Treat
Immediate post‑void rinsing is key because the urine is freshly expelled and still rich in glucose. Waiting even 15 minutes lets the sugar settle on skin, increasing fungal adhesion.
If an infection does appear, start a topical azole (e.g., clotrimazole) for 3‑5 days. Most cases resolve quickly; only 1-2 % become severe enough to need oral therapy.
When to Call a Doctor
Most genital mycotic infections are mild, but rare complications demand urgent care. Fournier's gangrene-a necrotizing fasciitis of the perineum-has been reported in 1.9 per 10,000 patient‑years. Signs include:
- Severe, spreading redness or blackening of skin
- Intense pain that feels out of proportion to the visible rash
- Foul odor or discharge
- Fever or chills
If any of these appear, seek emergency care immediately.
Putting It All Together: A Practical Checklist
- Start SGLT2 therapy with a 5‑minute counseling session from your diabetes team (ADA recommendation).
- Keep a water bottle at hand - sip regularly to hit the 2‑3 L goal.
- After each bathroom visit, rinse the genital area with water; repeat before bedtime.
- Wear breathable cotton underwear; change it daily.
- Avoid tight leggings, swim shorts, or leggings that trap moisture for more than a few hours.
- Carry a small reminder card with the rinsing steps; set a phone alarm for the night rinse.
- Document any irritation or infection in your logbook and tell your clinician at the next visit.
Following this routine helped a 2021 study cut infection rates by 40 % while keeping medication adherence above 90 %.
Frequently Asked Questions
Do I need to stop my SGLT2 inhibitor if I get a genital infection?
Usually not. Most infections are mild and respond to a short course of topical antifungal cream. Continue the medication unless infections become recurrent or severe, in which case your doctor may adjust the dose or switch drugs.
Can I use regular soap for genital cleaning?
Mild, unscented soap is acceptable, but the best practice is plain water. Harsh soaps or alcohol‑based wipes can irritate the skin and actually increase infection risk.
Is there a difference in infection risk between men and women?
Yes. Women generally see higher rates (4-12 %) compared with men (2-5 %). Anatomical differences and the higher surface area of the vulva create more opportunities for Candida to grow.
How long should I continue the hygiene routine after stopping the drug?
Maintain good genital hygiene as a general health habit. Even without glucosuria, moisture and friction can cause irritation, so the rinsing habit remains beneficial.
What are the signs of a serious infection like Fournier's gangrene?
Rapidly spreading redness, intense pain, foul odor, fever, or skin discoloration. Treat as an emergency - go to the ER immediately.
By combining proper hygiene, adequate hydration, and timely cleaning, you can keep the benefits of SGLT2 inhibitor genital infections low while still enjoying lower blood sugar, weight loss, and heart‑health protection.




Post A Comment