Hashimoto’s thyroiditis isn’t just another thyroid issue-it’s the most common reason people end up with hypothyroidism in countries like Australia, the US, and Canada. If you’ve been told your TSH is high, your energy is gone, and your weight won’t budge no matter what you do, this might be why. It’s not laziness. It’s not bad diet. It’s your immune system turning against your thyroid. And once you understand how TSH works, managing it becomes less like guesswork and more like a clear path forward.
What Exactly Is Hashimoto’s Thyroiditis?
Hashimoto’s thyroiditis is an autoimmune disease. That means your body’s defense system-designed to fight off viruses and bacteria-mistakes your thyroid gland for an invader. It sends antibodies to attack it. Over time, this constant assault damages the thyroid’s ability to make hormones. The result? Hypothyroidism: your body doesn’t get enough thyroid hormone to keep your metabolism, brain, heart, and muscles running right.
The condition was first described in 1912 by Japanese doctor Hakaru Hashimoto. Today, it accounts for about 90% of all hypothyroidism cases in places where people get enough iodine in their diet. In the US, roughly 4% of adults have it. Women are five to ten times more likely to develop it than men. It often shows up between ages 30 and 50, but it can strike at any time.
You don’t need to have symptoms to have Hashimoto’s. Many people are diagnosed after a routine blood test shows a high TSH. Others only notice things like fatigue, dry skin, constipation, or brain fog after months-or years-of feeling "off." The good news? Once diagnosed, it’s one of the most predictable and treatable endocrine conditions out there.
How Is It Diagnosed?
Diagnosis starts with a simple blood test: TSH. That’s thyroid-stimulating hormone, made by your pituitary gland. When your thyroid isn’t making enough hormone, your pituitary kicks into overdrive and pumps out more TSH to try and force the thyroid to work harder. So a high TSH is the first red flag.
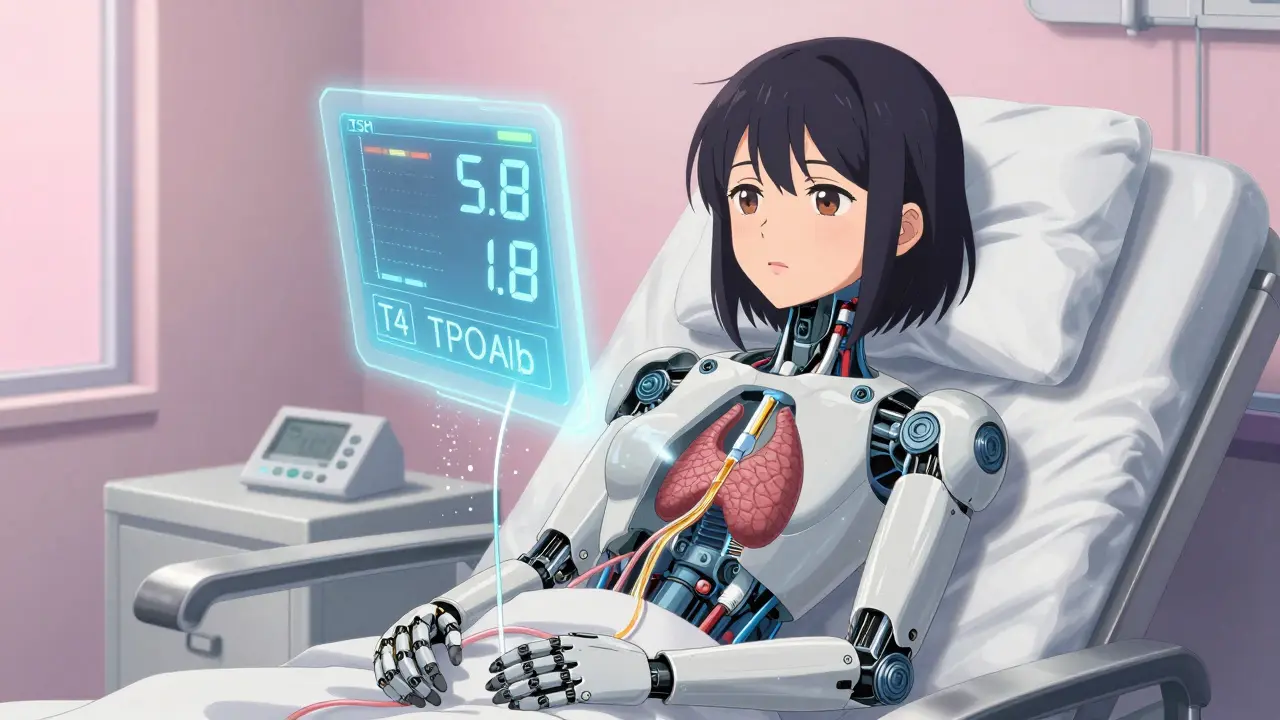
If your TSH is above 4.5 mIU/L, doctors will check two more things: free T4 (the active thyroid hormone in your blood) and thyroid peroxidase antibodies (TPOAb). If your T4 is low or low-normal and your TPOAb is high (usually above 35 IU/mL), you’ve got Hashimoto’s.
Here’s what that looks like in real numbers:
- TSH: 5.8 mIU/L (high)
- Free T4: 0.8 ng/dL (low-normal)
- TPOAb: 120 IU/mL (elevated)
That’s a classic Hashimoto’s profile. You don’t need to test T3 levels unless something unusual is going on. And you don’t need to retest antibodies later-those levels don’t change how you’re treated. The antibodies are just the signature of the disease, not the target of treatment.
Why TSH Is the Only Test You Need for Monitoring
This is where things get simple-and where most confusion comes from. Once you’re on levothyroxine (LT4), the only blood test you need regularly is TSH. Not T4. Not T3. Not antibodies. Just TSH.
Why? Because your pituitary gland is exquisitely sensitive to thyroid hormone levels. Even tiny changes in your free T4 will cause your TSH to shift. That makes TSH the most reliable indicator of whether your dose is right.
Major medical groups agree on this. The American Thyroid Association, the American Association of Clinical Endocrinologists, the Cleveland Clinic, and the Royal Australian College of General Practitioners all say: if you have primary hypothyroidism (not a pituitary problem), TSH alone is enough to guide your treatment.
Some patients ask, "But I still feel tired even though my TSH is normal." That’s common. And it doesn’t mean your dose is wrong. It might mean you need to aim for the lower end of normal-between 0.4 and 2.5 mIU/L-especially if you’re under 65. Studies show people with certain gene variations (like DIO2 polymorphisms) feel better with TSH targets in that lower range.
Don’t chase perfect numbers. Chase how you feel. But use TSH to guide the journey.
Starting Levothyroxine: What to Expect
Levothyroxine is a synthetic version of T4, the main hormone your thyroid makes. It’s safe, effective, and cheap. Generic versions work just as well as brand-name Synthroid-thanks to stricter FDA manufacturing rules since 2018.
Dosing isn’t one-size-fits-all. For most adults, doctors start with 1.4 to 1.8 mcg per kilogram of body weight. So if you weigh 70 kg (about 154 lbs), that’s roughly 100 mcg per day. But if you’re older, have heart disease, or have only mild hypothyroidism, you might start lower-25 to 50 mcg per day.
It takes time to find your sweet spot. Most people need 2 to 3 dose adjustments before they’re stable. That’s normal. Don’t get discouraged if your first dose doesn’t fix everything.
How Often Should You Get Tested?
Timing matters. TSH doesn’t change overnight. Levothyroxine has a long half-life-about 7 days. Your body needs 6 to 8 weeks to fully adjust to a new dose and for your pituitary to respond.
Here’s the standard timeline:
- Start levothyroxine.
- Wait 6 to 8 weeks.
- Get your TSH tested.
- If TSH is still high, increase dose by 12.5 to 25 mcg.
- Wait another 6 to 8 weeks. Test again.
- Repeat until TSH is in target range.
Once you’re stable, you only need a TSH test once a year. Some doctors will check every 6 months at first, especially if you’re new to treatment or have other health issues.
But here’s the catch: if anything changes in your life, you need to test sooner. That includes:
- Starting or stopping birth control pills, estrogen, or testosterone
- Beginning iron, calcium, or proton pump inhibitors (like omeprazole)
- Losing or gaining more than 10% of your body weight
- Becoming pregnant
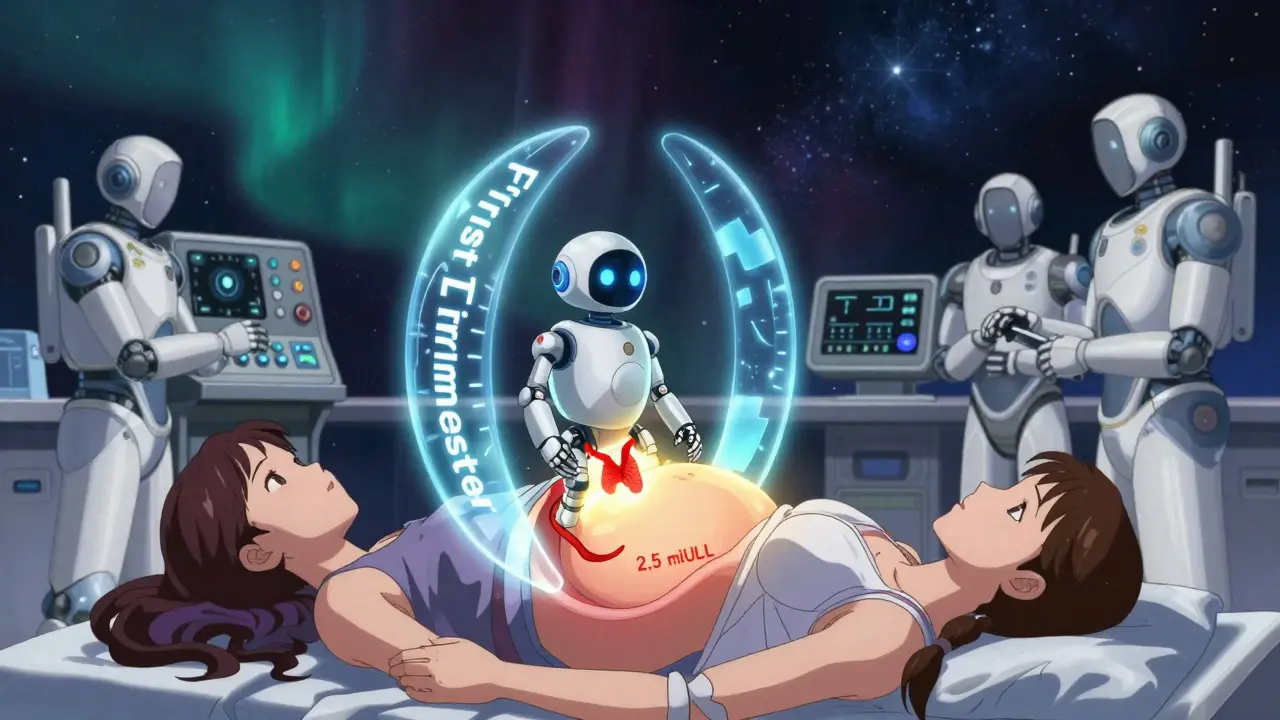
During pregnancy, TSH targets get tighter. If you have Hashimoto’s and are pregnant, your doctor will check TSH every 4 weeks until week 20. The goal? Keep TSH below 2.5 mIU/L in the first trimester. Why? High TSH during pregnancy increases the risk of miscarriage and preterm birth.
What If You Still Feel Bad Even With Normal TSH?
This is the biggest frustration for patients. You’ve done everything right. Your TSH is 1.8. Your doctor says you’re fine. But you’re still exhausted. Your hair is thinning. Your mood is off.
Here’s what to do:
- Ask your doctor to target the lower end of normal: 0.4 to 2.5 mIU/L.
- Check for other issues: low iron (ferritin), vitamin D, B12, or cortisol.
- Make sure you’re taking levothyroxine correctly-on an empty stomach, 30 to 60 minutes before food or coffee.
- Don’t take it with calcium, iron, or antacids-they block absorption.
Some people wonder about adding T3 (liothyronine) to their regimen. The Cochrane Review in 2022 looked at 11 studies involving over 1,500 people. It found no consistent benefit. The standard remains: levothyroxine alone, with TSH as the guide.
What You Can Do Right Now
If you’ve just been diagnosed:
- Write down your symptoms: fatigue, weight gain, cold intolerance, brain fog, dry skin, constipation.
- Take your medication at the same time every day, ideally in the morning before breakfast.
- Keep a simple journal: note how you feel each week. Did your energy improve? Did your mood lift? Did your hair stop falling out?
- Don’t skip your 6- to 8-week follow-up test. That’s your roadmap.
If you’ve been on treatment for a while:
- Review your last TSH result. Is it in the 0.4-2.5 range?
- Check if anything in your life changed recently-meds, weight, stress, sleep.
- If you’re feeling off, don’t assume it’s your thyroid. But don’t ignore it either. Request a TSH test.
What’s New in 2026?
Science keeps moving. In 2023, a major study of over 12,000 people found that those with certain genetic variants respond better to lower TSH targets. That’s pushing doctors to think more individually.
Pregnancy guidelines are also being updated. New recommendations suggest even tighter targets during each trimester:
- First trimester: TSH < 2.5 mIU/L
- Second trimester: TSH < 3.0 mIU/L
- Third trimester: TSH < 3.0 mIU/L
Home TSH tests are now FDA-approved. But they’re not yet recommended for routine use. Lab tests are still more accurate, especially at the low end of the scale.
And while some patients swear by gluten-free diets or selenium supplements to "calm" their immune system, there’s no strong evidence they change the course of Hashimoto’s. Stick to the proven path: TSH-guided levothyroxine.
Final Thoughts: You’re Not Broken
Hashimoto’s thyroiditis isn’t a failure. It’s not your fault. It’s not something you can "fix" with better willpower or a juice cleanse. It’s a medical condition with a clear, well-researched treatment plan.
The key isn’t perfection. It’s consistency. Take your pill. Get your TSH tested. Adjust as needed. And remember: your symptoms matter. If you feel better when your TSH is 1.2 instead of 3.8, that’s not "off-label." That’s personalized medicine.
You’re not alone. Millions of people live full, active lives with Hashimoto’s. You can too.



Post A Comment