Black Box Warning Risk Assessment Tool
Patient Risk Assessment Tool
This tool helps healthcare providers evaluate whether the benefits of a drug with a black box warning outweigh the risks for specific patients. Based on factors like age, pregnancy status, and comorbidities.
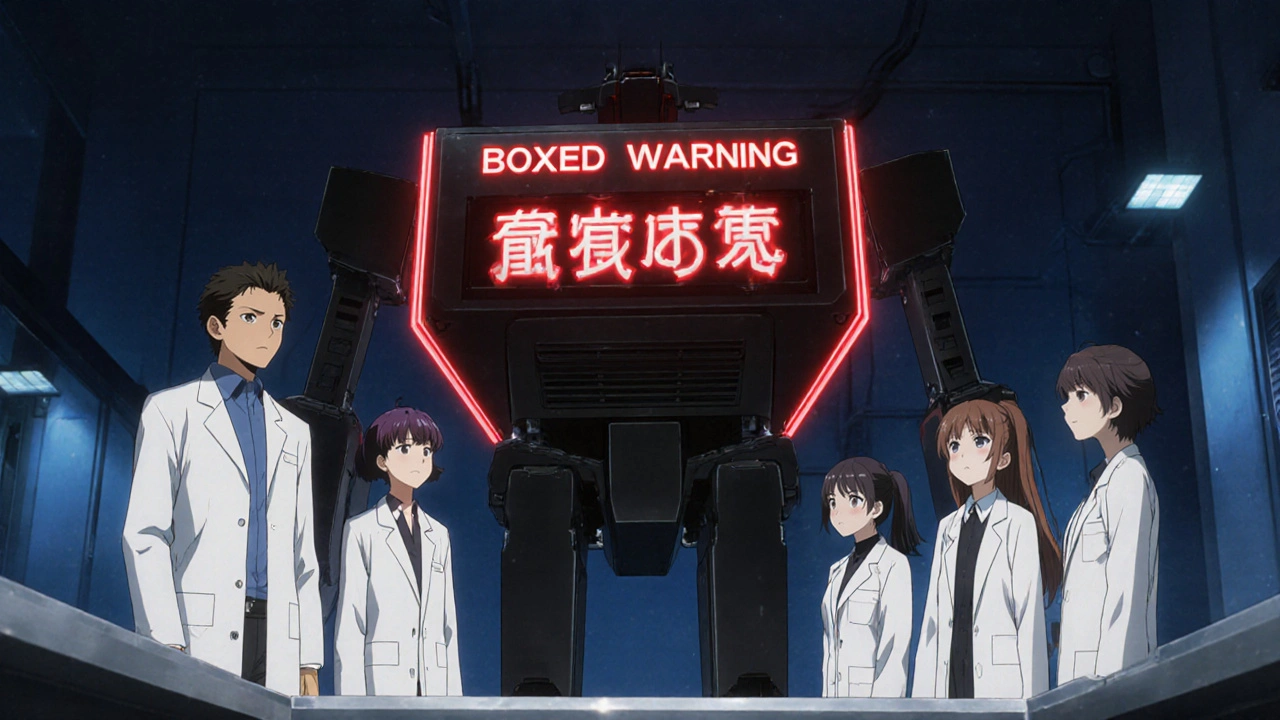
When a medication carries a FDA black box warning, also called a boxed warning, it signals the most serious safety alert the agency can issue. These warnings sit in a black border on the label, demanding a double‑take from anyone who reads the prescribing information.
What Exactly Is a Black Box Warning?
A black box warning is a regulatory requirement under the Federal Food, Drug, and Cosmetic Act. The rule lives in 21 CFR 201.56 and 201.57, which dictate the size, placement, and wording of the box. The warning appears near the top of the drug’s package insert, right after the Highlights of Prescribing Information section, so it can’t be missed.
How Does the FDA Decide to Add One?
The agency follows a multi‑stage review process. First, clinical trial data are examined for signals of life‑threatening adverse events. After a drug hits the market, the FDA Adverse Event Reporting System (FAERS) collects millions of reports each year, many of which are submitted through MedWatch. If patterns emerge that suggest a serious risk-such as severe liver injury, fatal heart rhythm problems, or birth defects-the FDA convenes an advisory committee, reviews the data, and may issue a boxed warning.
The decision hinges on three questions:
- Is the risk potentially fatal or causing permanent damage?
- Can careful monitoring or specific patient selection reduce the risk?
- Do the benefits still outweigh the risks for at least a subset of patients?
If the answer is yes to the first and the agency feels clinicians need to weigh the balance every time they prescribe, a black box warning is added.
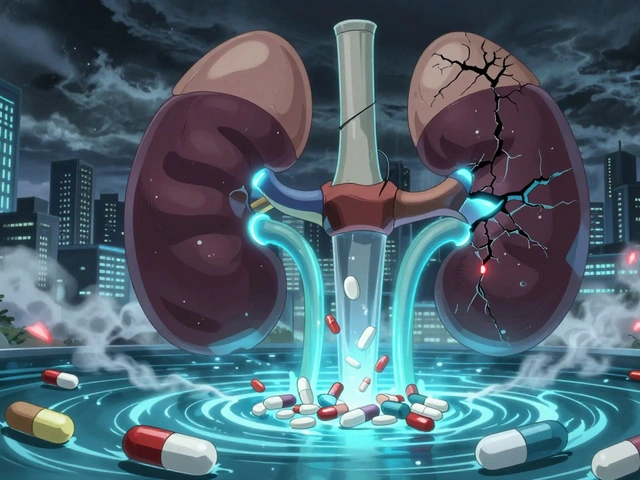
What Types of Risks Trigger a Black Box Warning?
The FDA groups risks into a few broad categories:
- Fatal or life‑threatening events - e.g., anaphylaxis, severe hemorrhage, cardiac arrest.
- Irreversible organ damage - e.g., hepatotoxicity, nephrotoxicity, optic nerve loss.
- Severe congenital anomalies - drugs that can cause birth defects when taken in pregnancy.
- Serious psychiatric effects - including suicidal ideation and severe depression.
- Complex monitoring requirements - drugs that need frequent lab tests, ECGs, or imaging to stay safe.
When a drug falls into any of these buckets, the agency drafts a warning that’s as direct as possible.

Impact on Prescribing Behavior
Studies show that a new black box warning can cut prescription rates dramatically. After the FDA added a warning to the diabetes drug rosiglitazone, prescriptions fell by roughly 70 %. The drop wasn’t universal-about 3.8 million patients kept using the drug because it was the only option for their condition. The warning acted like a traffic signal: it slowed the flow, but didn’t always stop it.
Clinicians often use the STEPS framework-Safety, Tolerability, Effectiveness, Price, Simplicity-to decide whether a drug with a warning is worth prescribing. If the safety profile is unacceptable for a given patient, the doctor looks for alternatives or adds a Risk Evaluation and Mitigation Strategies (REMS) program, which may require special certification, patient registries, or restricted dispensing.
Real‑World Examples You Might Recognize
Here are three well‑known drugs and the warnings that changed how they’re used:
| Drug | Primary Risk | Resulting Action |
|---|---|---|
| Isotretinoin (Accutane) | Severe birth defects | iPLEDGE program, mandatory pregnancy testing |
| Fluoroquinolones (e.g., ciprofloxacin) | Tendon rupture, aortic dissection | Prescribed only for serious infections, warned against use in older adults |
| Thalidomide (Revlimid) | Teratogenicity, neuropathy | Restricted distribution, REMS, mandatory counseling |
Each case illustrates that a boxed warning doesn’t ban a drug; it forces a more thoughtful approach.
What Patients and Providers Should Do
When you see a black box warning, follow this checklist:
- Read the warning word‑for‑word. It’s there to flag the most serious danger.
- Ask about monitoring. Do you need regular blood tests, imaging, or heart checks?
- Discuss alternatives. If another drug offers the same benefit with a lower risk, that may be preferable.
- Confirm REMS requirements. Some drugs need you to enroll in a patient registry or see a certified prescriber.
- Report side effects. Use MedWatch or your pharmacist to add your experience to FAERS.
Open communication is the only way the warning serves its purpose.
Future Directions: Precision and Digital Labeling
The FDA’s 2023‑2027 strategic plan mentions “enhancing the utility of drug labeling, including boxed warnings, through incorporation of pharmacogenomic information.” In plain English, that means the agency hopes to attach genetic risk data to the warning. If a certain allele makes a patient 10 times more likely to develop a severe reaction, the warning could say, “Patients with CYP2D6 *4 allele face heightened risk.”
Another frontier is digital labeling. Imagine a smart EMR that pulls the latest boxed warning text and highlights the sections most relevant to a patient’s comorbidities at the moment of prescribing. That could cut the lag between new safety data and bedside action.
Until those technologies become routine, the black box remains a static, high‑visibility box on paper and on the FDA’s Drugs@FDA website. Its purpose hasn’t changed: make sure the most dangerous risks are impossible to overlook.
Quick Reference Cheat Sheet for Clinicians
- Location: Directly after Highlights of Prescribing Information.
- Format: Black border, bold heading “Boxed Warning.”
- Key Content: Description of risk, patient populations at greatest danger, monitoring steps, and any REMS requirements.
- Action Step: Discuss each bullet with the patient before signing any prescription.
FDA black box warnings are not scare tactics; they are a safety net built on decades of data, intended to keep both doctors and patients from unintended harm.
What does a black box warning look like on a drug label?
The warning appears in a solid black border, usually right after the “Highlights of Prescribing Information” section. It contains a bold heading that reads “Boxed Warning” followed by a concise description of the serious risk.
Can a drug lose its black box warning?
Yes. If new clinical data show the risk is lower than originally thought, the FDA can remove or downgrade the warning. This usually requires robust post‑marketing studies or meta‑analyses.
Do all patients need to be warned about a boxed warning?
The warning is on the label for every patient, but clinicians tailor the discussion. For example, a pregnancy‑related warning is emphasized only for women of child‑bearing age.
How can I report an adverse reaction linked to a black box warning?
Use the FDA’s MedWatch portal, call 1‑800‑FDA‑1088, or tell your pharmacist. The report feeds into FAERS, helping the agency monitor safety trends.
What is a REMS program and why is it tied to some boxed warnings?
REMS (Risk Evaluation and Mitigation Strategies) are additional safety measures that may require special training for prescribers, patient enrollment, or restricted dispensing. They’re added when monitoring alone isn’t enough to keep patients safe.



Post A Comment