Itchy, red, watery eyes that won’t go away? You’re not alone. Around 40% of people in the U.S. deal with eye allergies every year, especially during spring and fall when pollen counts spike. Unlike pink eye caused by viruses or bacteria, eye allergies aren’t contagious-they’re your body’s overreaction to things like grass, dust, or pet dander. The result? Intense itching, swelling, and that frustrating burning feeling that makes it hard to focus on work, drive, or even sleep.
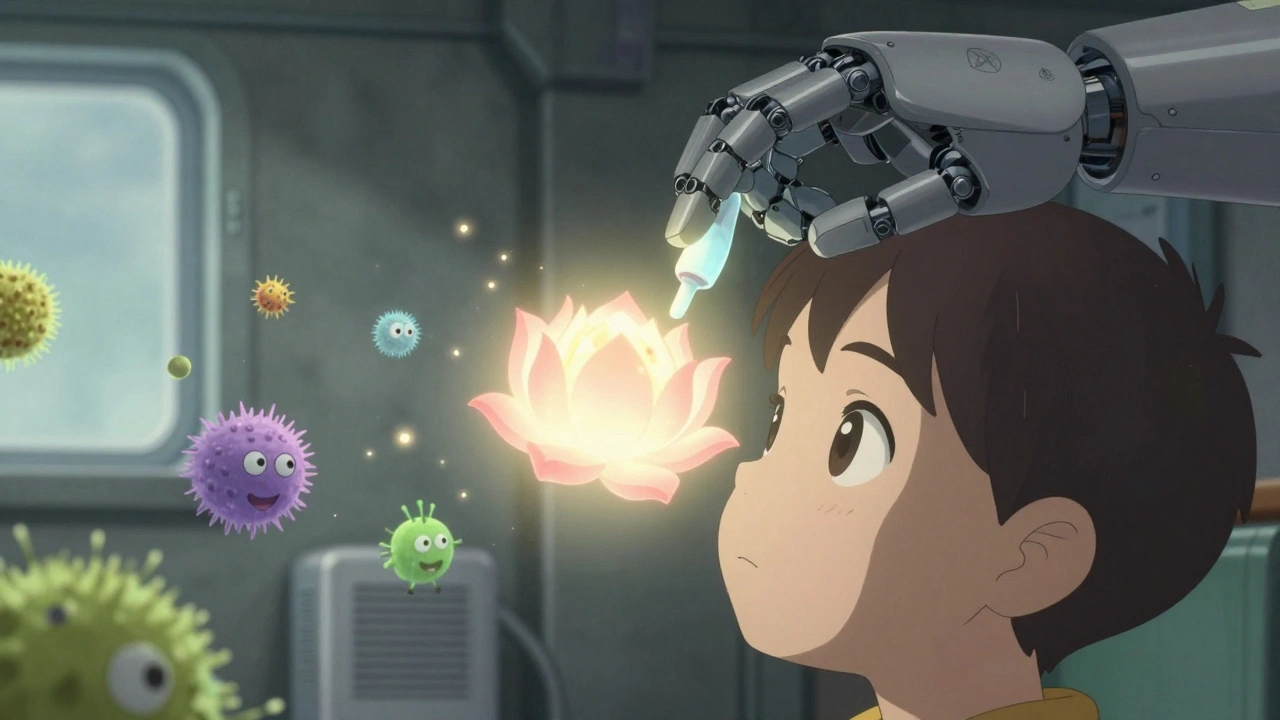
What’s Really Happening in Your Eyes?
Your eyes have a thin, clear membrane called the conjunctiva that covers the white part and lines the inside of your eyelids. When allergens like pollen land on it, your immune system goes into overdrive. Mast cells in the conjunctiva release histamine-the same chemical that causes sneezing and runny noses. That histamine triggers blood vessels to swell (redness), leaks fluid into tissues (swelling), and fires up nerve endings (itching). It’s a fast reaction: symptoms can show up in as little as 5 minutes after exposure.According to a 2023 study in Ocular Immunology and Inflammation, 92% of people with eye allergies report itching as their worst symptom. Redness follows close behind at 88%, with 85% dealing with watery eyes. Swollen eyelids and sensitivity to light are common too. The good news? This isn’t an infection. There’s no yellow or green discharge-just clear tears and relentless irritation.
Antihistamine Eye Drops: Your Fastest Relief
When it comes to quick relief, antihistamine eye drops are the go-to. They block histamine from binding to receptors in your eyes, stopping the itch before it starts. But not all drops are the same.First-generation drops like Naphcon-A (pheniramine) work fast-often within 3 to 5 minutes-but you have to use them every 4 to 6 hours. Many people complain about stinging when they apply them, and the relief doesn’t last long.
Second-generation drops like olopatadine (Pataday), ketotifen (Zaditor, Alaway), and epinastine (Elestat) are better. They don’t just block histamine-they also stabilize mast cells, so fewer allergens trigger the reaction in the first place. This dual action means longer-lasting relief. Pataday Once Daily Relief, for example, reduces itching scores by over 75% and lasts up to 16 hours. In clinical trials, users went from severe itching (score of 2.8 on a 4-point scale) down to barely noticeable (0.7) within just 3 minutes.
Generic ketotifen costs around $13 for a 2.5mL bottle. Brand-name Pataday runs closer to $43. Insurance often covers the prescription version at a $15-$40 copay. For many, the extra cost is worth it: fewer applications, better control, and less disruption to daily life.
What About Other Treatments?
You might be tempted to grab Visine-A or another redness-reliever. But here’s the catch: decongestant drops like tetrahydrozoline shrink blood vessels to reduce redness-but they cause rebound redness if used more than 3 days in a row. A 2023 study found 65% of users developed worse redness after a week of daily use. That’s not relief-it’s a cycle you can’t escape.Oral antihistamines like Zyrtec or Claritin help with sneezing and nasal symptoms, but they dry out your eyes. About 40% of users report increased dryness and irritation, which can make eye allergies feel even worse. If you’re already dealing with dry eyes, these aren’t the best choice.
Mast cell stabilizers like cromolyn sodium (Crolom) are great for prevention but useless if you wait until symptoms start. You need to use them 2-4 days before pollen season hits. That’s fine if you know your triggers and timing-but not helpful when you’re already in the middle of a flare-up.
For severe cases, doctors may prescribe steroid eye drops like loteprednol. These work fast, but they’re not for everyday use. Long-term use raises your risk of glaucoma and cataracts. Only use them under strict supervision and for short periods.

What Experts Recommend
Leading allergy and eye specialists agree: the best first-line treatment for moderate to severe eye allergies is a combination antihistamine/mast cell stabilizer. Dr. David A. Grieshaber, an ophthalmologist in Switzerland, calls ketotifen and olopatadine the “gold standard.” The American College of Allergy, Asthma & Immunology (ACAAI) specifically recommends olopatadine 0.2% (Pataday Once Daily) because of its 16-hour duration and proven effectiveness.But here’s something many people miss: how you apply the drops matters just as much as which one you pick. A 2022 study in Ophthalmology Times found that half of patients don’t use eye drops correctly. The trick? Tilt your head back, pull down your lower eyelid to make a little pocket, and drop the medicine into that space-not directly onto the eyeball. Don’t let the bottle touch your eye. That keeps it clean and reduces infection risk.
Also, don’t blink right after applying. Close your eyes gently for 30 seconds. That gives the medicine time to spread over the surface.
Real People, Real Results
On Reddit, users in the r/allergies community shared over 1,200 experiences with eye allergy treatments. Nearly 70% said Pataday worked best for severe symptoms. Many wrote things like: “Works within minutes and lasts all day.” But cost came up often: “I love it, but I can’t afford it without insurance.”On Amazon, Zaditor got 4.1 stars. Users liked the price but said they had to reapply midday. One review said: “Great value, but I’m using two bottles a month.”
And then there are the bad experiences. One Drugs.com user wrote: “Used Visine-A for 5 days straight and my eyes got worse than ever.” That’s rebound hyperemia in action. It’s not just ineffective-it makes things worse.
One of the most successful stories? A Reddit user who combined Pataday in the morning with cold compresses. Within 48 hours, their symptoms went from unbearable to manageable.
What You Can Do Right Now
Medication helps-but it’s not the whole story. The most effective approach combines treatment with prevention:- Wash your face and hands after being outside-especially during high pollen seasons. This cuts allergen exposure by about 30%.
- Use preservative-free artificial tears 4-6 times a day. They rinse allergens off your eyes and soothe irritation.
- Wear wraparound sunglasses outdoors. A 2023 trial showed they block up to 50% of airborne pollen.
- Keep windows closed during peak pollen hours (usually 5 a.m. to 10 a.m.). Use air conditioning instead.
- Change your pillowcase every 2-3 days. Dust mites love them.
When to See a Doctor
If you’ve been using antihistamine drops correctly for 2 weeks and your eyes are still itchy, red, or swollen, it’s time to see an eye doctor. About 20% of people who think they have allergies actually have dry eye disease, blepharitis, or another condition that looks similar. Treating the wrong problem makes things worse.Also, if you notice changes in vision, pain, or thick discharge, don’t wait. Those aren’t allergy symptoms-they could signal infection or something more serious.
The Future of Eye Allergy Treatment
The eye allergy market is growing fast, valued at $1.8 billion in 2023. New treatments are on the horizon. In September 2023, the FDA approved bepotastine besilate 1.5% (Bepreve) as a once-daily option. Ocular Therapeutix is testing a tiny insert that fits in the tear duct and releases medication for up to 3 months. Biologics targeting specific inflammation pathways (like IL-4 and IL-13) are in early trials.But here’s the big picture: pollen counts have risen 21% since 1990, and climate change is making allergy seasons longer and stronger. The ACAAI predicts eye allergies will affect 40% more people by 2035. That means better, longer-lasting treatments aren’t just nice to have-they’re becoming essential.
Right now, the best thing you can do is pick the right drop, use it correctly, and pair it with simple environmental changes. You don’t need to suffer through every spring and fall. With the right tools, your eyes can stay clear, calm, and comfortable.





Post A Comment