Medication Comparison Tool
Compare Your Medication Options
Enter your medication choices to see how they compare in benefits and side effects based on what matters most to you.
What matters most to you in your treatment?
Why switching meds isn’t just a doctor’s call
Changing medications isn’t like swapping out a battery. One pill might ease your symptoms, but it could also make you gain weight, feel dizzy, or mess with your sleep. And if you switch to another, you’re not guaranteed it’ll be better - you might just trade one problem for another. That’s why more doctors and patients are turning to decision aids before making a switch. These aren’t fancy apps or marketing brochures. They’re structured tools that lay out the real numbers: how likely you are to benefit, how likely you are to suffer a side effect, and what your options actually look like side by side.
What a decision aid actually shows you
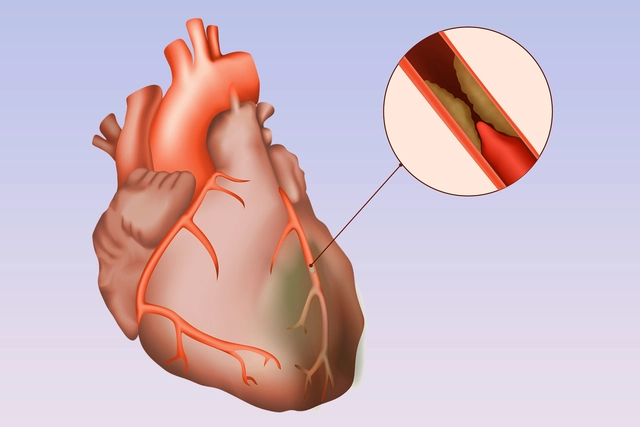
Forget vague phrases like “this drug has few side effects.” Real decision aids give you hard numbers. For example, if you’re considering switching from warfarin to a DOAC for blood thinning, you’ll see something like: “Out of 100 people like you, 8 will have a serious bleed on warfarin over 5 years. On the new drug, it’s 3.” That’s not a guess. That’s based on studies tracking thousands of patients.
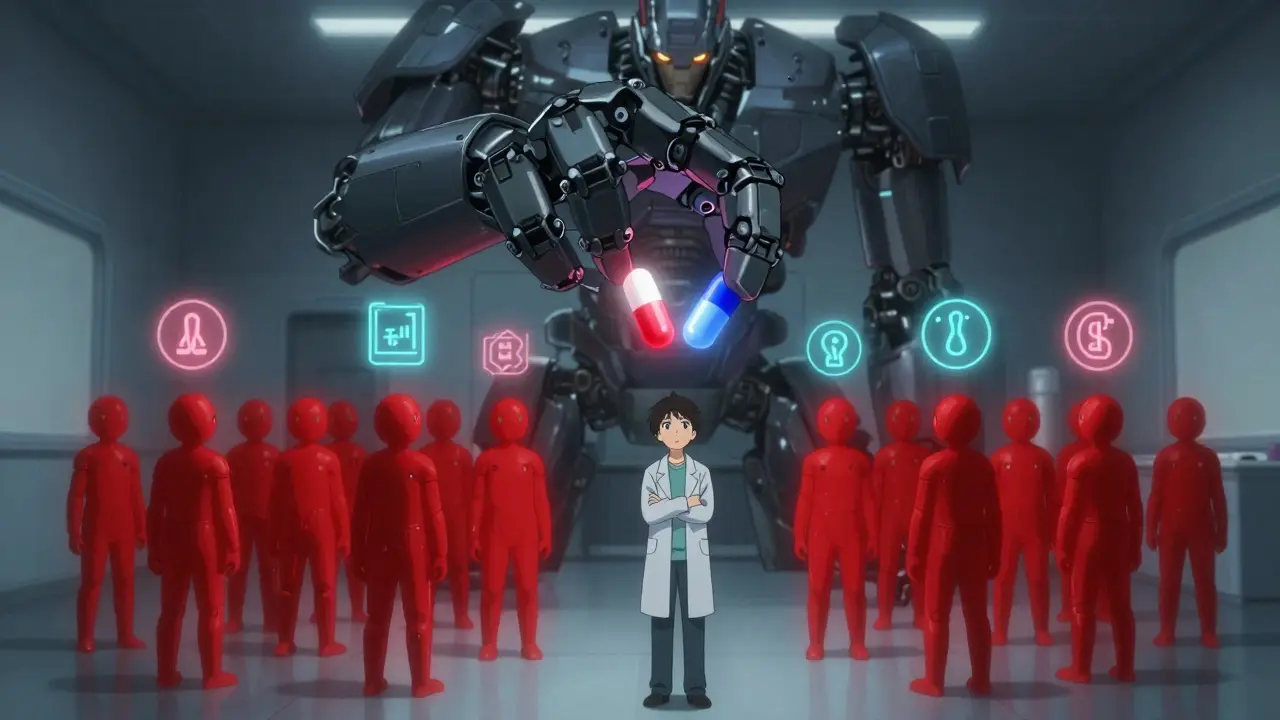
These tools use visual icons - little pictures of people, some colored red to show side effects - so you can see the risk without doing math. You might see 100 tiny figures. Three are red for bleeding risk on the new drug. Eight are red on the old one. Suddenly, it’s not abstract. It’s real. And it’s personal.
It’s not just about side effects - it’s about what matters to you
One person hates taking pills multiple times a day. Another is terrified of weight gain. A third can’t afford a drug that costs $500 a month. A good decision aid doesn’t just list risks. It asks you: What’s most important to you?
You’ll be asked to rank things like:
- How much does dosing frequency matter?
- Is avoiding a rare but scary side effect worth a higher cost?
- Can you live with fatigue if it means fewer hospital visits?
There’s no right answer. But when you see your values reflected in the options, you’re less likely to quit the drug later because it “felt wrong.” Studies show that when patients use these tools, they’re 28% less likely to feel conflicted or regretful about their choice.
How this beats the old way of talking
Traditionally, a doctor might say: “We’re switching you to this. It’s better.” Or worse: “It’s your choice, but I think this one’s best.” Neither gives you real clarity.
Decision aids change that. A 2022 review found patients using them remembered 32% more about their options six months later than those who just got a pamphlet. They didn’t just hear facts - they processed them. They compared. They thought. That’s why, in VA hospitals, 78% of patients say they felt more confident in their medication decisions after using these tools.
One Reddit user wrote: “The icon array showing 100 people with 3 bleeding events on the new drug versus 8 on the old one made it real for me.” That’s the power of seeing it visually, not just hearing it.
When decision aids don’t work - and why
These tools aren’t magic. They don’t help if you’re in a crisis. If your blood pressure spikes or you’re having a panic attack, you need a quick fix, not a 20-minute interactive tool.
They also struggle when the information is too complex. A 2022 study found no benefit for patients with cognitive impairment (MMSE score below 24). And some people just get overwhelmed. In one Mayo Clinic study, 31% said they felt buried in numbers. That’s why good decision aids are designed to be used before the appointment - not during a rushed 10-minute visit.
Another problem? Not all tools are created equal. Some downplay serious risks. The FDA issued 12 warning letters in 2023 to developers who minimized side effects or made benefits sound guaranteed. Always check if the tool comes from a trusted source - like the VA, Mayo Clinic, or the Ottawa Hospital Research Institute.
How to use one - step by step
If your doctor suggests switching meds, ask: “Is there a decision aid for this?” Here’s how to make it work:
- Get the tool ahead of time. Most are web-based or sent via patient portal. Don’t wait until the appointment.
- Use it alone first. Read it. Watch the videos. Play with the sliders. Let it sink in.
- Write down your top concerns. “I can’t handle weight gain.” “I need something cheap.” “I’m scared of bleeding.”
- Bring your notes to the appointment. Say: “I used the tool. Here’s what stood out to me.”
- Ask: “Which option matches what I said matters most?”
Doctors who use these tools regularly say the conversation shifts from “I think you should” to “What do you want?” That’s the whole point.
Who’s using these tools - and who isn’t
They’re common in mental health, heart care, and diabetes clinics - places where choices are complex and side effects matter a lot. In VA hospitals, 68% of clinics use them for antidepressants and anticoagulants.
But in regular primary care? Only 29% do. Why? Time. A 2023 study found it adds 7-12 minutes to a visit. Most doctors don’t have that. But after using them 10 times, the extra time drops to under 5 minutes. Training helps. The AHRQ offers free 4-hour modules for clinicians.
There’s also a financial push. Medicare Advantage plans now get bonus payments for using shared decision-making tools. That’s why adoption is growing - not because it’s trendy, but because it’s now financially smart for health systems.
What’s next for decision aids
The next wave is personalization. Intermountain Healthcare launched an AI tool in early 2024 that adjusts how risks are shown based on how you learn. If you prefer pictures, it shows icons. If you like numbers, it gives percentages. If you’re anxious, it tones down the scary stats.
The FDA is also stepping in. In 2024, they proposed new rules requiring decision aids to be tested on real patients - including older adults, non-English speakers, and people with low health literacy - before they’re used in clinics. That’s a big step toward fairness and accuracy.
Bottom line: You deserve to know what you’re signing up for
Switching meds shouldn’t feel like a gamble. You’re not just choosing a drug. You’re choosing how you’ll feel, how much you’ll pay, and what risks you’re willing to live with. Decision aids don’t make the choice for you. They just give you the facts, clearly, honestly, and in a way that matches what matters to you.
If your doctor hasn’t offered one, ask. If they say no, ask why. And if you’re switching because you’re fed up with side effects - don’t just quit. Use a tool. Find out what else is out there. Your next pill might be better - but only if you know exactly what you’re trading.
Are decision aids only for serious illnesses?
No. Decision aids are used for any medication switch where there’s more than one good option - even for things like antidepressants, blood pressure pills, or diabetes drugs. It’s not about how serious the illness is, but whether the choices have different trade-offs. If two drugs both work but have different side effects, a decision aid helps you pick the one that fits your life.
Can I use a decision aid without my doctor’s help?
You can look at one on your own, but they’re designed to be used with your doctor. The tool gives you facts, but your doctor helps you interpret them in the context of your health history. Using it alone might help you ask better questions, but skipping the conversation means you could miss important details - like drug interactions or how your kidney function affects dosing.
What if I don’t understand the numbers?
That’s normal. Decision aids use icons, simple language, and comparisons to make numbers easier. If you’re still confused, say so. Ask your doctor to explain using real-life examples: “If 100 people took this drug, how many would have this side effect?” Don’t pretend you get it just to move on. The goal is for you to feel sure - not overwhelmed.
Do these tools cost money?
No. Most are free and provided by hospitals, government programs, or universities. The VA, Mayo Clinic, and Ottawa Hospital all offer theirs at no cost. Be wary of apps or websites asking for payment - legitimate decision aids are public health tools, not products to sell.
What if I use the tool and still feel unsure?
That’s okay. Decision aids don’t force a choice. If you’re still unsure, it’s a sign you need more time or more information. Ask your doctor if you can schedule a follow-up. You can also ask for a second opinion. Making a medication change is a big decision - and it’s fine to take your time.
Can decision aids help me avoid bad side effects?
Yes - that’s one of their biggest strengths. Many patients use them to avoid switching to a drug that causes a side effect they’ve had before or deeply fear. One patient declined a switch to a new diabetes drug after seeing a 15% chance of pancreatitis. That’s not a rare fear - it’s a real risk. The tool helped them say no confidently, avoiding a potentially dangerous outcome.



Post A Comment