Coordinated Specialty Care: What It Is and How It Helps People with Early Psychosis
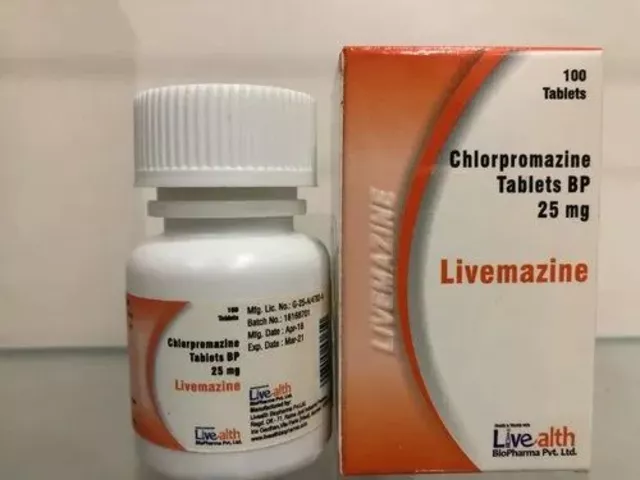
When someone first shows signs of psychosis—like hearing voices, feeling paranoid, or losing touch with reality—time matters. Coordinated specialty care, a structured, team-based approach designed specifically for people experiencing early psychosis. Also known as CSC, it’s not just another therapy—it’s a full support system built to stop psychosis from taking over someone’s life. Unlike traditional care that hands you a pill and sends you on your way, coordinated specialty care brings together doctors, therapists, case managers, and peer specialists who work as one team. They don’t just treat symptoms—they help you get back to school, work, and relationships.
This model doesn’t just focus on medication. It includes family education, training for loved ones to understand psychosis and respond with support, not fear, cognitive behavioral therapy, a practical way to challenge confusing thoughts and reduce distress, and supported employment or education, helping people return to daily routines without pressure. Studies show people in coordinated specialty care are twice as likely to stay in treatment, hold a job, and avoid hospitalization compared to those getting standard care. It’s not magic—it’s structure, consistency, and human connection.
You won’t find this kind of care everywhere yet, but it’s growing. Many programs are tied to hospitals, community clinics, or state mental health networks. If you or someone you know is in the early stages of psychosis, asking for coordinated specialty care isn’t asking for special treatment—it’s asking for the best chance to recover. Below, you’ll find real stories and practical guides on how this approach works, what medications help, how families get involved, and how to spot warning signs before things get worse. These aren’t theory pieces—they’re tools from people who’ve been there.